
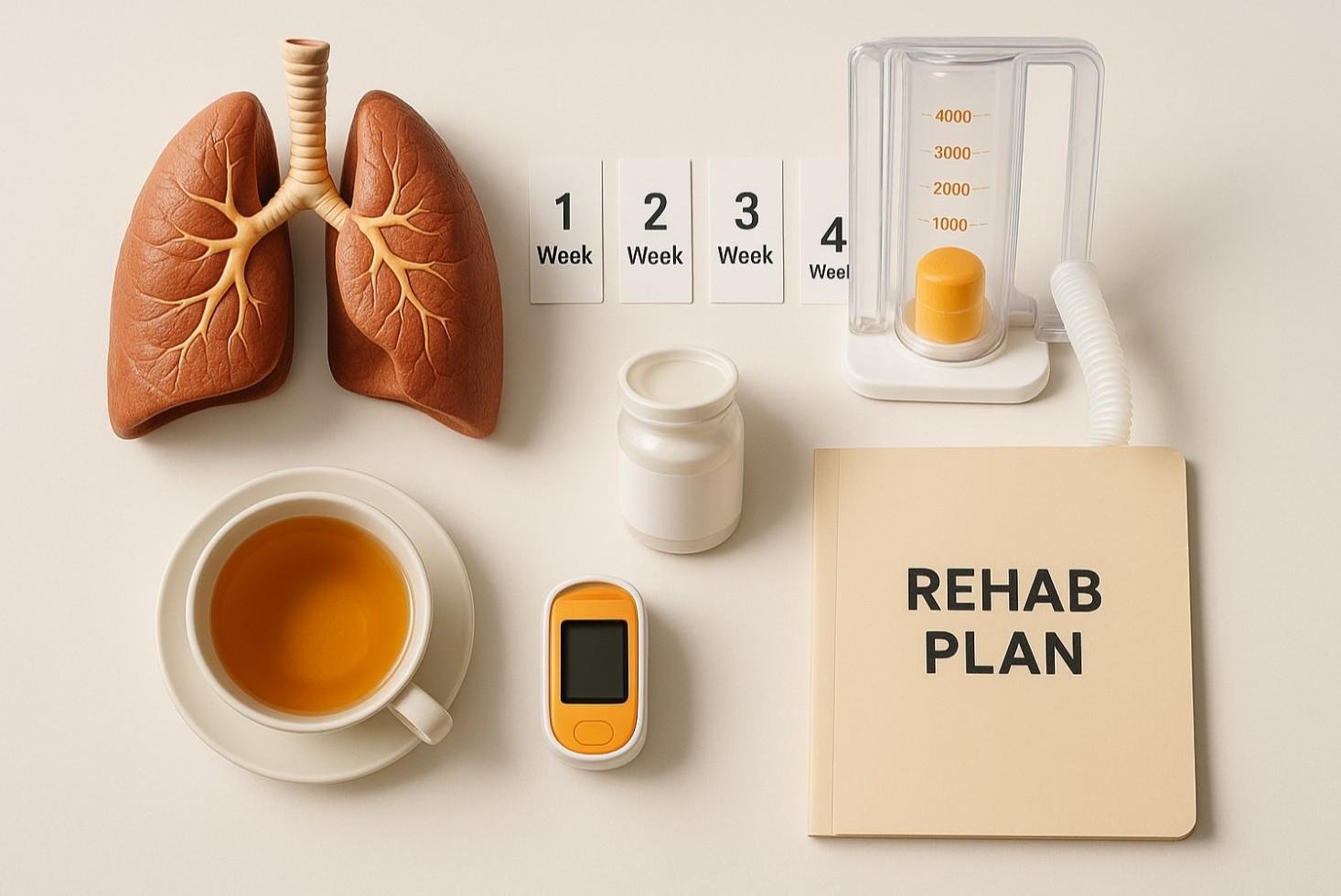
Minimally invasive Lung Cancer Surgery (VATS or Robotic) involves removing lung tumors through small incisions using cameras and precision instruments. Unlike open surgery, patients typically walk within 24 hours, discharge in 3–4 days, and return to light daily activities within 3 to 4 weeks.
If you or a loved one has just undergone Lung Cancer Surgery, the hardest part is technically over. The tumor is out. But now you’re facing the "what next?" phase.
At Chest Surgery India, we often see patients who expect to be bedridden for months. That is the old way. With modern Video-Assisted Thoracoscopic Surgery (VATS) and Robotic surgery, the game has changed completely. You aren't just "recovering" — you are actively retraining your body.
This guide is written to give you a clear, no-fluff timeline of what happens from the moment you wake up in the recovery room to the day you get back to your everyday life.
There is a massive misconception that "recovery" means "rest."
Actually, recovery implies movement.
The biggest mistake we see patients make is staying in bed too long. When you lie flat, your lungs don't expand fully. This creates a playground for pneumonia. We need you up, moving, and developing those lungs immediately.
According to 2024-2025 clinical protocols, early mobilization (walking within 24 hours) reduces post-operative complications by over 30%. It’s not just good advice; it’s a medical necessity.
Day 0: The Wake-Up Call
You will wake up groggy. You’ll likely have a chest tube on one side to drain fluid and air. It’s uncomfortable, but it’s doing a vital job.
Days 1–3: The Work Begins
This is where the "lung training" starts. You will be given a small plastic device called a Spirometer.
This One Habit Will Speed Up Your Healing
When you get home, your energy will crash. This is normal. Your body is burning massive calories to heal the internal staple lines.
Don't aim for one long walk. Aim for "micro-walks." Walk for 10 minutes every 2 hours inside your house. This keeps your blood moving without exhausting you.
For our patients in India, this is a non-negotiable safety rule. Do not use a squat-style toilet. Squatting increases pressure in your abdomen and chest, which can stress your healing incisions. Use a Western-style commode or a chair riser for at least 4 weeks.
To help you understand why your recovery feels faster than stories you might have heard from the past, look at this comparison.
| Feature | Traditional Open Surgery | Minimally Invasive (VATS/Robotic) |
| Incision Size | 6–10 inches (Ribs spread) | 1–2 inches (No rib spreading) |
| Hospital Stay | 5–8 Days | 2–4 Days |
| Pain Level | High (Requires strong meds) | Low to Moderate |
| Return to Work | 2–3 Months | 3–4 Weeks |
| Risk of Infection | Higher | Significantly Lower |
The "Danger Zone" of Feeling Better
By Week 2, you might feel good enough to pick up a grocery bag or lift a grandchild. Don't do it.
You might feel a burning sensation or numbness near the incision. This is not a complication; it is the nerves "waking up" and regenerating. It usually fades on its own.
Forget the "sick diet" of plain rice and dal water. You need protein to build cells.
Return to Driving and Work
Life after Lung Cancer Surgery involves follow-up scans to ensure you remain cancer-free. This anxiety is real. We recommend sticking to a strict surveillance schedule—usually a CT scan every 6 months for the first two years. Knowing you are being watched closely is the best antidote to fear.
Q: When can I fly after surgery?
Most patients can fly 3–4 weeks post-surgery, once the chest X-ray confirms there is no air leak. Always check with us before booking.
Q: Can I do Yoga?
Yes, but modify it. Anulom Vilom (breathing) is great immediately. Avoid Kapalabhati (forceful exhaling) for at least 3 months as it puts high pressure on the chest.
Q: Is Robotic surgery more expensive?
While the upfront cost is higher, recent data suggests the total cost of care often balances out because you spend fewer days in the hospital and return to work faster.

18+ Yrs Exp | 5,700+ Thoracic & Robotic Cancer Surgeries
Dr. Parveen Yadav is a Director and Senior Consultant in Thoracic and Surgical Oncology, specializing in minimally invasive and robotic lung and esophageal surgeries, with advanced training from AIIMS and Tata Memorial Hospital.
View Full Profile Pain After Thoracic Surgery: Tips for Smooth Recovery
Pain After Thoracic Surgery: Tips for Smooth Recovery
 Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
 Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures
Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures
Struggling with pain after chest surgery? Dr. Parveen Yadav shares expert recovery tips, causes of shoulder pain, PTPS signs, and what your discharge sheet won't tell you.
Discover how diet, breathing exercises & daily habits help prevent and recover from thoracic cancer. Expert insights from Dr. Parveen Yadav, Chest Surgery India
Discover how Da Vinci robotic surgery is transforming chest procedures in Gurgaon. Less pain, faster recovery & expert care by a certified thoracic surgeon
Copyright 2026 © Dr .Parveen Yadav all rights reserved.
Proudly Scaled by Public Media Solution!