
If you or a loved one has just been told you need lung surgery, you are likely feeling overwhelmed. It’s a stressful diagnosis, and it’s followed by a confusing set of choices. You are probably hearing terms like "Open Thoracotomy," "VATS," and "Robotic Surgery," all while trying to process what this means for your health, your family, and your finances.
My name is Dr. Parveen Yadav. As a thoracic surgeon with over 18 years of experience, including specialized training in surgical oncology at AIIMS, New Delhi, and a fellowship in thoracic surgery at Tata Memorial Hospital, Mumbai, I have performed all three types of these operations. My goal with this guide is to cut through the confusion.
You have two big, immediate questions:
Let's answer those questions with transparent, honest, and up-to-date information for 2025.
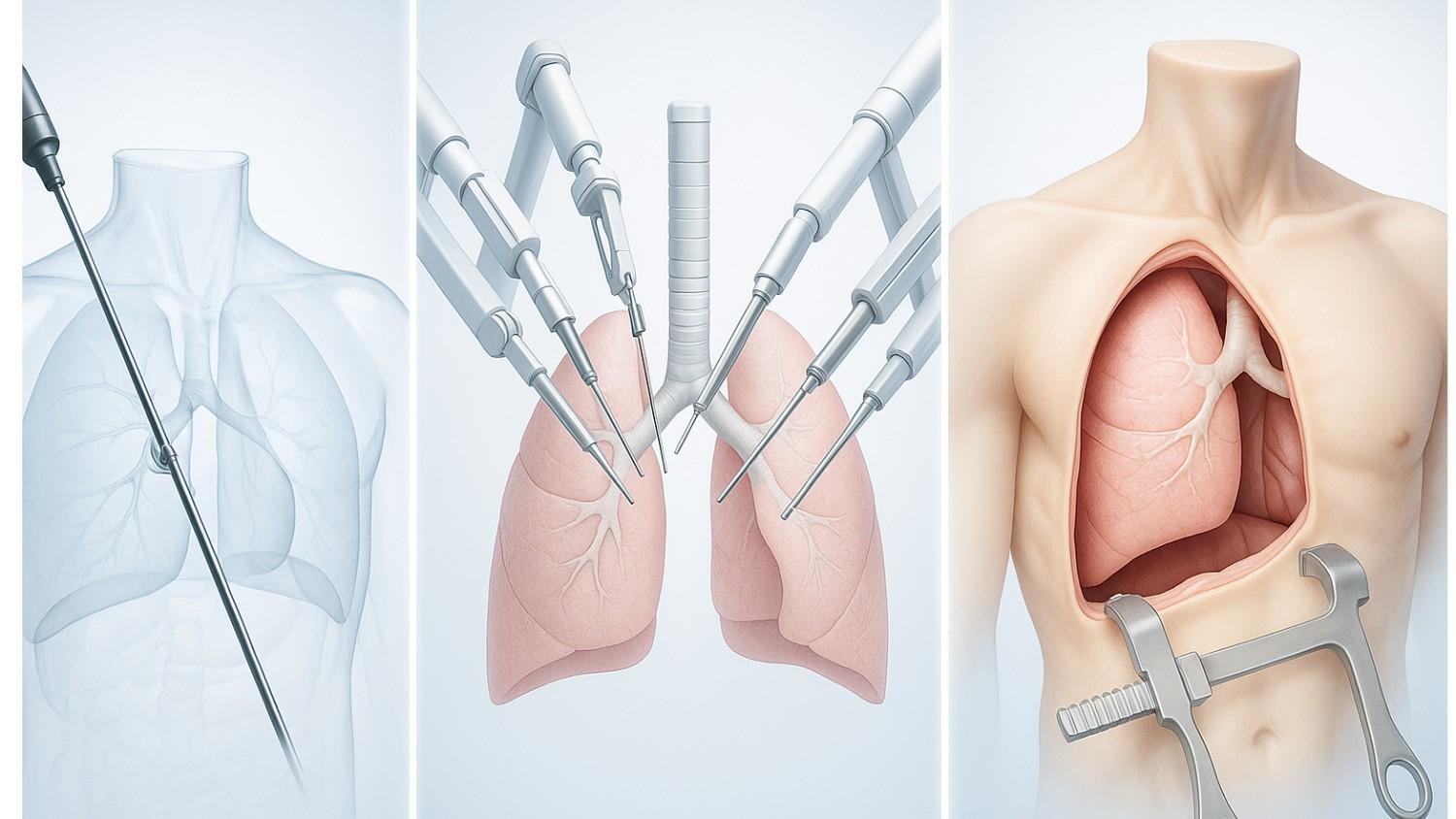
Before we talk about cost and recovery, let's quickly define what these procedures are. The goal for all three is often the same—to remove the cancerous part of the lung (a procedure called a lobectomy). The only thing that changes is the tool the surgeon uses to get there.
This is the surgery your parents or grandparents would have had. To reach the lung, the surgeon makes one long incision (often 15-20 cm) on the side of your chest. The most crucial part to understand is that this procedure requires the ribs to be manually spread apart with a retractor to give the surgeon space to work. This rib-spreading is the primary source of the significant post-operative pain and longer recovery associated with this surgery.
This is the modern "keyhole" or "minimally invasive" standard. Instead of one large cut, the surgeon makes 3-4 small incisions (or "ports"), each just a few centimeters long. A tiny high-definition camera and long, rigid instruments are placed through these ports. The surgeon performs the entire operation by watching a 2D monitor.
The biggest benefit? The ribs are not spread. This directly translates to less pain, less tissue damage, and a much faster recovery.
This is the most advanced "keyhole" approach and an evolution of VATS. It uses 3-4 small incisions, just like VATS.
Here’s the difference: the surgeon sits at a nearby console, controlling a set of robotic arms. This system gives the surgeon two game-changing advantages over VATS:
For many patients, seeing the data side-by-side is the most helpful. This table summarizes the key differences based on current data.
| Feature | Open Thoracotomy | VATS (Keyhole) | RATS (Robotic) |
| Est. Procedure Cost (India) | ₹2,70,000 - ₹5,95,000 | ₹1,60,000 - ₹3,20,000 | ₹7,50,000 - ₹12,50,000 |
| Typical Hospital Stay | 7 - 14 days | 3 - 5 days | 3 - 5 days |
| Typical Return to Work | 4 - 6 weeks+ (~27 days) | 2 - 3 weeks (~12.5 days) | 2 - 3 weeks |
| Post-Operative Pain | Very High (due to rib spreading) | Low | Potentially Lowest |
| Intra-Op Blood Loss | High | Low | Lowest |
| Scarring | Large 15-20cm scar | Minimal (3-4 small scars) | Minimal (3-4 small scars) |
| Risk of "Conversion-to-Open" | N/A | Higher (6.6% - 11.0%) | Lowest (0.7% - 6.0%) |
| Lymph Node Dissection | Good | Good | Excellent (Superior Staging) |
| Long-Term Cancer Survival | Equivalent | Equivalent | Equivalent |
The table shows a huge cost difference. Let's break down why.
There is no ambiguity here: RATS is the most expensive option. This is not due to the surgeon's fee; it is due to the technology itself.
These costs are passed on to the patient, making the upfront price of the procedure significantly higher.
This is the most important financial concept I discuss with my patients. Many people look at the table and see that Open Thoracotomy (starting at ₹2,70,000) looks cheaper than Robotic Surgery and sometimes VATS.
This is a dangerous oversimplification. You must look at the "Total Cost of Care."
An open surgery's lower procedure cost is often canceled out by its recovery cost.
The Takeaway: When you factor in the shorter hospital stay and faster return to work, VATS is often the most affordable and highest-value option for the patient.
This is what matters most to your quality of life. The difference in recovery is not small—it is profound.
This is the "black box" of Indian healthcare, and it causes families immense stress. You must be your own advocate here.
The good news is that the Insurance Regulatory and Development Authority of India (IRDAI) has mandated that insurers must cover "modern treatments," which includes robotic surgeries.
BUT... this does not mean they will pay the full amount. Insurers use three common "traps" to limit their payout:
Do not schedule your surgery until you have written pre-authorization from your insurer. Call your TPA (Third-Party Administrator) and ask these three questions:
Getting these answers in writing before your admission is the most critical piece of financial advice I can give you.
As your surgeon, my priority is curing your cancer. This is where the technical details matter.
Let me put your biggest fear to rest. For early-stage lung cancer, high-quality studies show that Open, VATS, and Robotic surgery all have equivalent and excellent long-term cancer survival rates.
The choice is not about if we can cure cancer. The choice is about the path (the pain, recovery, and risk) we take to get that cure.
So, if survival is the same, why ever pay for the expensive robot? As a surgeon, RATS gives me two significant technical advantages, which translate into tangible patient benefits.
You've seen the data. VATS offers incredible value. RATS offers the pinnacle of technology. Open surgery is the proven, traditional method.
So, what should you choose?
My honest advice is this: The expertise of your surgeon is more important than the tool in their hand.
I have seen this my entire career. An expert, high-volume VATS surgeon will always get a better, safer result than a novice surgeon using a robot for the first time. The robot does not do the surgery; I do the surgery. The robot is a tool that enhances my skills.
The ideal scenario is to find a surgeon who is an expert in all three techniques. This ensures their recommendation is based 100% on your specific tumor, your anatomy, and your needs—not on the only procedure they know how to do.
When you go for your consultation (or second opinion), you are empowered with this information. Ask your surgeon these direct questions :
There is no single "best" surgery. There is only the best surgery for you.
If you or a loved one is facing a lung surgery diagnosis and are seeking a clear, comprehensive second opinion, I am here to help. Please contact my office in Delhi or Gurgaon. We will sit down together, review your scans, and create a clear, personalized plan to get you through this.

18+ Yrs Exp | 5,700+ Thoracic & Robotic Cancer Surgeries
Dr. Parveen Yadav is a Director and Senior Consultant in Thoracic and Surgical Oncology, specializing in minimally invasive and robotic lung and esophageal surgeries, with advanced training from AIIMS and Tata Memorial Hospital.
View Full Profile Pain After Thoracic Surgery: Tips for Smooth Recovery
Pain After Thoracic Surgery: Tips for Smooth Recovery
 Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
 Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures
Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures
Struggling with pain after chest surgery? Dr. Parveen Yadav shares expert recovery tips, causes of shoulder pain, PTPS signs, and what your discharge sheet won't tell you.
Discover how diet, breathing exercises & daily habits help prevent and recover from thoracic cancer. Expert insights from Dr. Parveen Yadav, Chest Surgery India
Discover how Da Vinci robotic surgery is transforming chest procedures in Gurgaon. Less pain, faster recovery & expert care by a certified thoracic surgeon
Copyright 2026 © Dr .Parveen Yadav all rights reserved.
Proudly Scaled by Public Media Solution!