

It was a Tuesday afternoon in the OT at Artemis Hospital. A 54-year-old school teacher from Faridabad had just been wheeled out of the operating room. Her daughter was waiting outside, hands clasped, eyes red. She had spent three nights on the internet reading about open chest surgery — the long scar, the broken ribs, the weeks of pain, the months away from her classroom. When I walked out and told her that her mother's lung tumour had been removed through four tiny incisions smaller than her thumbnail, and that she would likely go home in two days, she just stared at me. Then she burst into tears. Not from fear. From relief she had not dared to feel until that moment.
That day stayed with me. Because her fear was real. For decades, chest surgery meant a 20-centimetre cut between the ribs, a hospital stay that stretched into weeks, and a recovery that robbed patients of months of their lives. That story has now changed. And the technology that changed it is called the Da Vinci Robotic Surgical System.
In this article, I want to walk you through what robotic thoracic surgery actually is, how it works inside the operating room, why it is different from older methods, what it can and cannot do, and why this matters deeply if you or someone in your family is facing a chest-related illness.
|

Let me clear one thing up first, because I hear this question every week from patients:
|
The Da Vinci system has three main parts. The first is the patient cart, which holds four robotic arms positioned around the patient. The second is the vision cart, which houses the 3D camera and energy systems. The third is the surgeon console, where I sit and control everything.
Here is what makes Da Vinci different from anything that came before it:
According to Intuitive Surgical, more than 14 million procedures have been performed globally using Da Vinci systems. Over 38,000 peer-reviewed research papers have studied its outcomes. This is not an experimental technology. It is the most researched surgical robot in the history of medicine.
Here is something that most articles about robotic surgery completely skip over, and I find it genuinely important.
The chest cavity is a naturally rigid, stable space. Unlike the abdomen, which is soft and can shift, the thoracic cage holds its shape. This creates consistent, predictable working space for the robotic arms. The narrow passages between lung lobes, blood vessels, airways, and lymph nodes are exactly where 7-degree wrist instruments perform at their best. Rigid laparoscopic tools struggle here. Robotic instruments do not.
Research published in leading thoracic surgery journals notes: 'The rigid anatomy of the chest appears to be an ideal condition for robotic-assisted surgery, enabling access to structures that are difficult or impossible to reach with standard video-assisted methods.' (Annals of Thoracic Surgery, 2022)
This is why robotic thoracic surgery has grown so rapidly. In 2009, robotic lobectomy represented less than 1% of all lobectomies performed in the United States. By 2020, that figure had risen to over 15% and continues to grow. The chest is where robotics deliver their highest value.
At our centre at Artemis Hospital, we use Da Vinci robotic surgery to treat a wide range of thoracic conditions. Patients travel from across India and abroad for these procedures. Many come after being told elsewhere that their surgery would require a large open incision.
Whether you are looking for an experienced oncologist in Gurgaon or seeking thoracic surgery in Delhi NCR for a second opinion, the range of robotic procedures available at our centre is comprehensive.
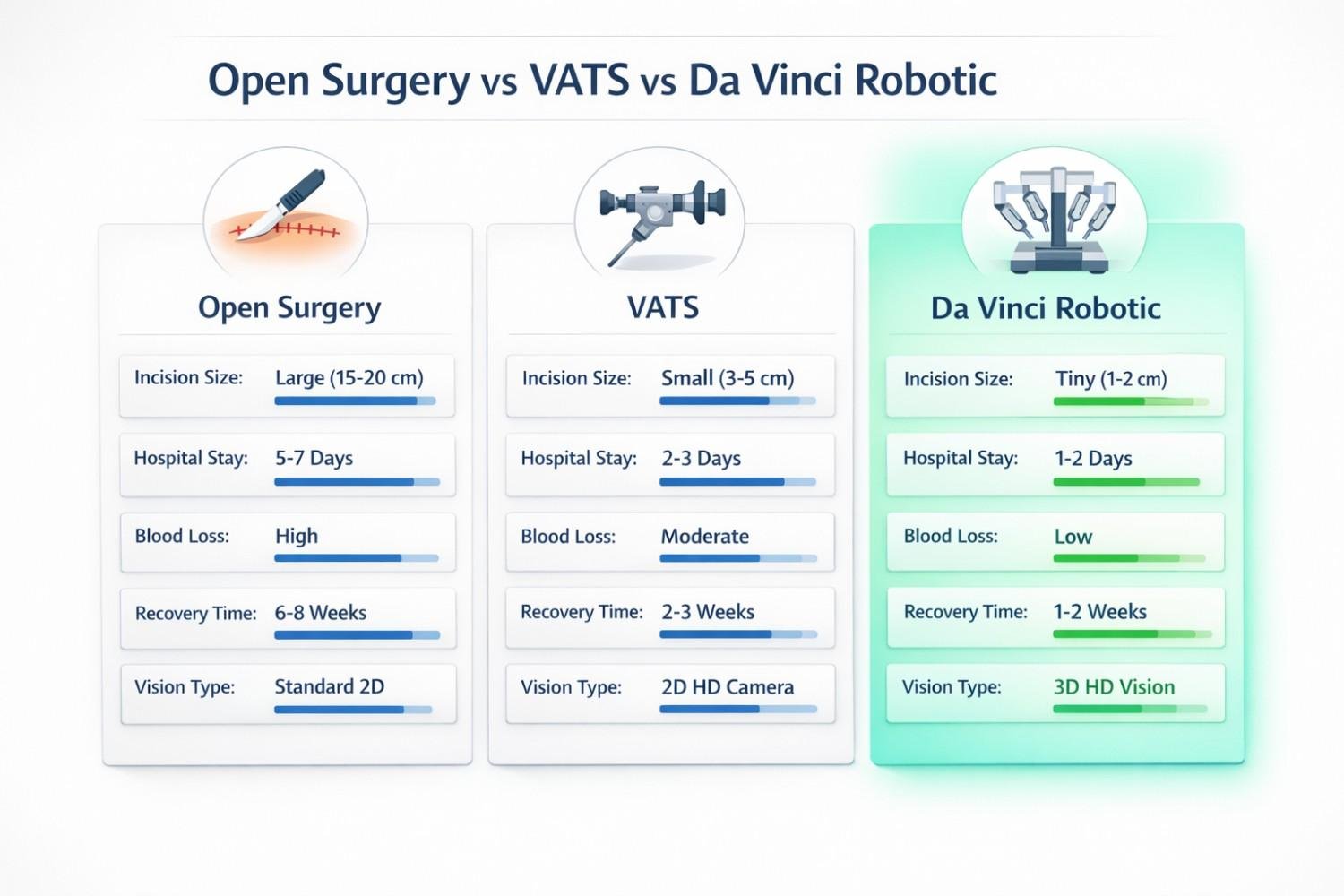
Every patient asks this question. Most websites avoid giving a straight answer. Here is the honest comparison based on published clinical data:
| Factor | Open Surgery | VATS | Da Vinci Robotic |
| Incision Size | 12 to 25 cm | 0.5 to 1.5 cm ports | 0.8 cm ports (4 to 5) |
| 3D Vision | Naked eye only | 2D flat camera | 3D HD, 10x magnification |
| Instrument Dexterity | Full arm movement | 4 degrees of freedom | 7 degrees of freedom |
| Blood Loss (avg.) | High | Moderate | Lowest (41% less vs VATS*) |
| Hospital Stay | 6 to 10 days | 3 to 6 days | 1 to 3 days (many cases) |
| Return to Normal Life | 6 to 12 weeks | 3 to 6 weeks | 2 to 4 weeks |
| Tremor Filtering | None | None | Yes, built-in |
| Lymph Node Removal | Good | Moderate | Most thorough of all three |
| Surgeon Fatigue | High (standing, bent) | High (standing, bent) | Low (seated console) |
*Source: PubMed comparative study on intraoperative blood loss in robotic vs. VATS lobectomy. Robotic average: 219 mL. VATS average: 374 mL.
|
This is something I rarely see discussed in patient-facing content, and I think that is a serious gap. Inside the Da Vinci system is a feature called FIREFLY, which uses a dye called ICG (Indocyanine Green) to light up invisible anatomy under near-infrared light.
When ICG is injected into the bloodstream, it glows bright green under infrared light at the surgeon's console. This makes blood vessels, lymph nodes, and tissue boundaries visible in ways that no other technology currently offers during live surgery.
Surgeons at Cleveland Clinic describe ICG fluorescence as 'surgical reassurance'. I would describe it as turning the lights on in a room you used to navigate in the dark.
I am going to be completely honest here, because I believe patients deserve the truth and not just a sales pitch.
Robotic surgery is not the right choice for every patient or every situation. A surgeon who tells you otherwise is not giving you the full picture.
|
| STAT | WHAT IT MEANS |
| 14M+ | Total Da Vinci procedures performed globally (Intuitive Surgical, 2024). |
| 38,000+ | Peer-reviewed studies validating Da Vinci surgical outcomes — the most researched robot in medical history. |
| 10x | Magnification of the Da Vinci 3D camera compared to the naked human eye. |
| 219 mL | Average blood loss in robotic lobectomy vs 374 mL in early VATS. A 41% reduction. (PubMed, comparative study.) |
| 1 to 3 | Days hospital stay in many robotic thoracic cases vs 6 to 10 days in open surgery. |
| 15%+ | Share of US lobectomies now performed robotically, up from less than 1% in 2009. (Society of Thoracic Surgeons, 2023.) |
Whether you are consulting an oncologist in Gurgaon, seeking thoracic surgery in Delhi, or getting a second opinion anywhere in the world, these questions matter:
A good surgeon will welcome every single one of these questions. If your surgeon seems impatient with them, that itself is important information.
Remember the school teacher from Faridabad I told you about at the beginning? She returned to her classroom six weeks after surgery. She sent me a photograph from her school's annual function. She was standing in front of her students, holding a small award they had made for her. A paper certificate that said, in a child's handwriting: 'Our favourite teacher, back again.'
Robotic thoracic surgery did not just remove a tumour from her lung. It gave her a future that felt whole. That is what this technology is really about. Not the robot. Not the console. Not the 3D camera or the 7-degree wrists. It is about patients leaving the hospital feeling like human beings, not like they have just survived a war.
Here is a quick summary of what we covered:
If you or someone you love is facing a chest surgery diagnosis, Dr. Parveen Yadav, Director of Thoracic Surgery and Surgical Oncology at Artemis Hospital, Gurgaon, offers consultations for patients seeking robotic thoracic surgery in Gurgaon and thoracic surgery in Delhi NCR. Whether you need a first opinion or a second one, the conversation is always worth having.
Are you ready to ask the right questions? If you are navigating a thoracic diagnosis right now, what is the one question you are most afraid to ask your surgeon? Reach out for a consultation. There are no wrong questions when it comes to your health. |

18+ Yrs Exp | 5,700+ Thoracic & Robotic Cancer Surgeries
Dr. Parveen Yadav is a Director and Senior Consultant in Thoracic and Surgical Oncology, specializing in minimally invasive and robotic lung and esophageal surgeries, with advanced training from AIIMS and Tata Memorial Hospital.
View Full ProfileDiscover how diet, breathing exercises & daily habits help prevent and recover from thoracic cancer. Expert insights from Dr. Parveen Yadav, Chest Surgery India
Just diagnosed with thoracic cancer? Learn critical first steps, biomarker testing, and what to do in the first 2 weeks from expert Dr Parveen Yadav.
Learn how advanced robotic surgery treats thymoma and esophageal cancer with greater precision, minimal invasion and improved recovery beyond lung-focused care.
Copyright 2026 © Dr .Parveen Yadav all rights reserved.
Proudly Scaled by Public Media Solution!