

Rajan was 54 years old when his routine chest X-ray showed something the radiologist quietly called suspicious. He had never touched a cigarette. He was not overweight. He ate home-cooked food most days. So when the diagnosis came back as early-stage lung cancer, his first reaction was complete disbelief. How? Why me?
Weeks later, Rajan sat across from his thoracic surgeon after a successful VATS lobectomy. He expected to hear about medicines, follow-up scans, and timelines. Instead, the surgeon leaned forward and asked something simple: “Tell me what you eat for breakfast. Do you walk? How well are you sleeping?”
That conversation changed everything for Rajan. He had assumed the battle against thoracic cancer was fought only inside an operation theatre. What he discovered is that the fight continues every single day, at the dining table, on the morning walk, and in the way you breathe. He is not alone in this discovery.
Your food choices, physical activity, sleep quality, and even the air inside your kitchen are all active players in both preventing thoracic cancer and recovering from it. This guide is written for patients, families, caregivers, and anyone who wants to understand the full picture of thoracic cancer care, including the parts that do not show up on a prescription.
Thoracic cancers are cancers that develop in the chest region. This includes lung cancer, esophageal cancer, cancer of the mediastinum (the space between the lungs), and chest wall tumors. Together, they are among the most serious cancers diagnosed today in India and globally.
Here is the surprising truth: smoking is not the only cause. Non-smoking women in India have one of the highest rates of lung cancer globally. Research consistently points to diet, indoor air pollution, excess body weight, and a sedentary lifestyle as major contributors.
Excess body weight is the second biggest lifestyle-related cancer risk factor after smoking. The good news is that these are factors you can actually change.
A diet that is high in red meat, processed foods, refined carbohydrates, and saturated fat is consistently linked to worse cancer outcomes in research. Alcohol is a proven carcinogen and is directly connected to esophageal cancer, even in people who have never smoked. Low intake of fruits and vegetables is itself an independent cancer risk factor, not just the absence of good nutrition.
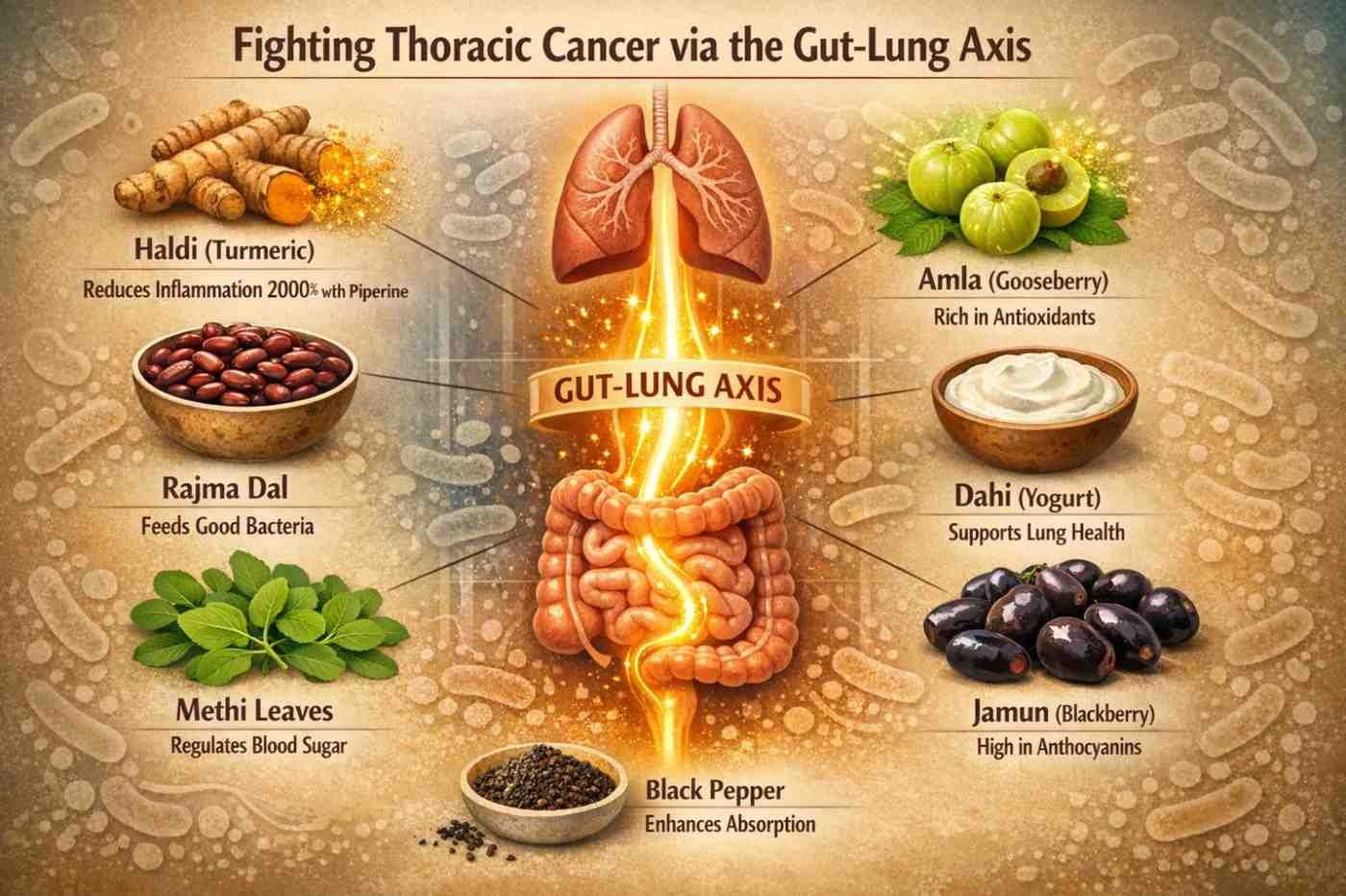
Here is where Indian cooking has a natural head start. The traditional Indian diet is rich in foods that science now confirms to have strong anti-cancer properties. The table below maps common Indian kitchen ingredients to their confirmed health benefits:
| Indian Food | Active Compound | Science-Backed Benefit |
|---|---|---|
| Haldi (Turmeric) | Curcumin | Reduces inflammation; may slow cancer cell growth via NF-kB and COX-2 inhibition |
| Amla (Indian Gooseberry) | Vitamin C, Polyphenols | Powerful antioxidant; supports immune surveillance |
| Rajma and Dal | Dietary Fiber, Plant Protein | Feeds beneficial gut bacteria; supports anti-tumor immunity |
| Dahi and Chaas | Probiotics | Maintains a healthy gut microbiome; critical for lung immune function |
| Methi (Fenugreek) | Soluble Fiber | Anti-inflammatory; supports gut health and hormone balance |
| Gobhi and Broccoli | Sulforaphane | Shown in studies to reduce cancer risk and support cellular repair |
| Berries and Jamun | Anthocyanins, Antioxidants | Mayo Clinic oncologists recommend a daily half-cup as a core cancer-prevention habit |
You have probably heard that turmeric prevents cancer. The reality is more nuanced, and getting this right actually matters for patient safety.
Lab studies published in Oncotarget do show that curcumin, the active compound in turmeric, can block cancer cell growth through multiple biological pathways. It reduces inflammation by acting on key molecular triggers. This is real science.
However, high-dose curcumin supplements may actually behave as a pro-oxidant in the oxygen-rich environment of the lungs, especially in ex-smokers, based on research reviewed on PubMed. The safe approach is to use turmeric as a food spice rather than in megadose capsule form. One practical tip: always add a pinch of black pepper when cooking with turmeric, since piperine increases curcumin absorption by up to 2000%, making your daily dal or sabzi far more effective than any supplement.
What most health websites do not tell you is this: your gut and your lungs are in constant, active communication. The bacteria living in your digestive system directly influence the immune cells that patrol your lungs.
Researchers call this the gut-lung axis. Think of it as a two-way information highway between your stomach and your chest. When your gut bacteria are diverse and healthy, your lungs receive stronger immune protection. When gut bacteria are damaged by poor diet, stress, or unnecessary antibiotics, your lungs lose that protection. This is not theory. It is actively shaping how cancer specialists now approach treatment.
Researchers at MD Anderson Cancer Center produced a result that is hard to ignore. Lung cancer patients who ate a high-fiber diet before immunotherapy had a 77% objective response rate. Patients in the low-fiber group, receiving the same immunotherapy treatment, had only a 29% response rate.
How does dietary fiber create this difference? Fiber feeds beneficial gut bacteria. Those bacteria produce compounds called Short Chain Fatty Acids (SCFAs). One specific SCFA called butyrate directly triggers cancer cell death and blocks the processes that help tumors grow, according to research published in Frontiers in Oncology. SCFAs also provide energy to the cells lining your intestine and act as anti-inflammatory messengers throughout the body.
Most people do not connect their gut health to their lung health. These are the common habits that damage the gut microbiome the most:
| What Damages the Gut | The Consequence for Your Lungs |
|---|---|
| Unnecessary antibiotic use | Antibiotic use reduced immunotherapy survival by over 70% in several NSCLC studies |
| High-fat, high-sugar daily diet | Promotes inflammatory gut bacteria; weakens anti-tumor immune response |
| Chronic stress | Triggers gut dysbiosis; breaks down the gut-lung immune connection |
| Smoking | Directly alters gut bacteria composition, increasing harmful strains |
| Processed and packaged foods | Strips out fiber; starves the beneficial bacteria your lungs depend on |
Gut-friendly Indian foods to actively eat more of: dahi, chaas, sabja seeds, oats, rajma, amla, haldi-doodh with black pepper, and methi.
What most patients only discover after their surgery: what you eat and how active you are in the weeks BEFORE thoracic surgery directly affects how well and how quickly you recover.
This concept is called prehabilitation. Studies show that patients who followed a high-protein diet and a structured exercise routine before surgery had significantly shorter hospital stays and fewer post-surgical complications. The goal is straightforward: you want to walk into the operating theatre in the strongest possible nutritional state.
Focus on protein at every single meal. Protein preserves muscle mass, and that muscle is what heals your body after major chest surgery. Good protein sources accessible in Indian households include eggs, fish, chicken, paneer, dal, and curd. Layer in colorful vegetables, whole grains like daliya and oats, and drink plenty of water throughout the day.
The American Cancer Society recommends that nutrition screening begin immediately after diagnosis, not weeks later when treatment is already underway. Malnutrition going into surgery significantly raises complication risk.
If you are preparing for Robotic Thoracic Surgery in Gurgaon or any major thoracic procedure, discuss a prehabilitation nutrition plan with your surgical team well before your scheduled operation date.
Treatment for thoracic cancer, whether chemotherapy, radiation, immunotherapy, or surgery, creates very real eating challenges. Nausea, mouth sores, taste changes, and fatigue make it difficult to eat well. Here is a practical quick-reference guide:
| Side Effect | What Helps | What to Avoid |
|---|---|---|
| Nausea | Small meals every 2-3 hours; cold food; ginger tea | Strong smells; large portions; lying down after eating |
| Mouth Sores | Soft bland food; cold liquids; curd rice; khichdi | Spicy, acidic, or very hot food and drinks |
| Taste Changes | Marinated food; light spices; umami-rich options | Forcing foods that smell repulsive to you right now |
| Fatigue | Protein at every meal; oats or daliya for slow energy | Skipping meals; relying on sugary drinks for energy |
| Constipation | High-fiber fruits; prunes; papaya; adequate water | Depending only on medication without dietary change |
This is where many well-meaning patients and families get it wrong. High-dose antioxidant supplements, especially beta-carotene, Vitamin E, and Vitamin C in very large doses, can directly interfere with how chemotherapy and radiation work inside the body.
Clinical trials have shown that high-dose beta-carotene supplements actually increased lung cancer risk in smokers. The clear consensus from the American Cancer Society, Johns Hopkins, and MD Anderson is this: get your nutrition from food first. Never take supplements without first telling your oncologist, especially if you are undergoing active treatment.
The first and most important priority after lung surgery is simply getting enough calories into your body. Appetite is often reduced after anesthesia and major surgery, and that is completely normal. Do not aggressively restrict fat or salt in the first two months. Getting adequate calories in is the priority.
Focus on protein-rich foods such as eggs, fish, chicken, dal, and paneer to support tissue repair. Sip water consistently throughout the day since dehydration after thoracic surgery commonly causes fatigue, dizziness, and nausea that many patients do not link back to fluid intake.
Start walking as soon as your surgeon clears you. Even short walks around the room prevent dangerous post-surgical complications including blood clots and hospital-acquired pneumonia.
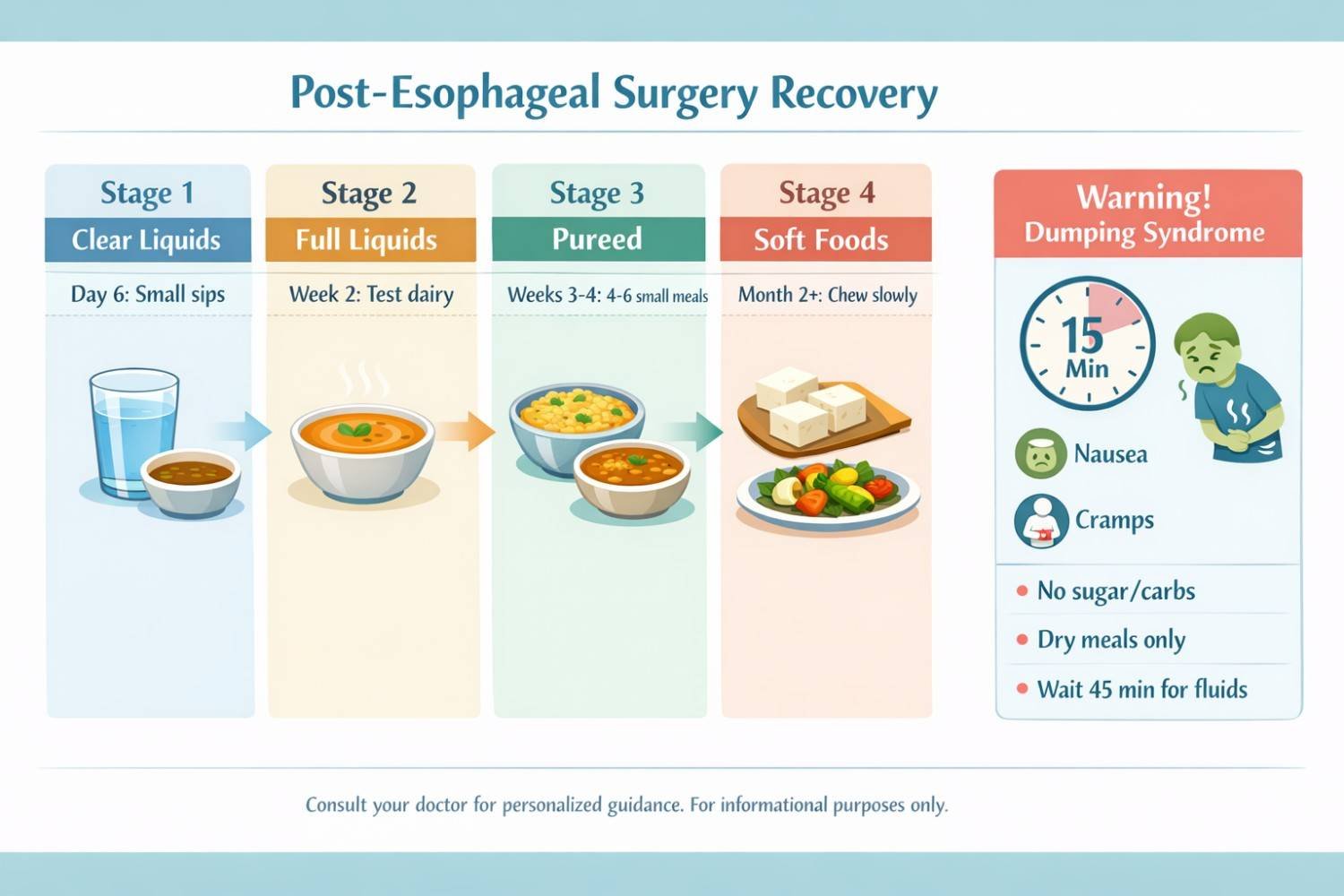
Esophageal surgery fundamentally changes how you can eat. Your stomach capacity shrinks dramatically. Many patients are discharged without a clear understanding of what this means for their daily meals. Here is the stage-by-stage plan:
| Stage | Timing | What You Can Eat | Key Rule |
|---|---|---|---|
| Stage 1: Clear Liquids | Day 6 post-surgery | Water, clear broth, diluted juice. No dairy yet. | Small sips only. 6-8 sessions daily. Never gulp. |
| Stage 2: Full Liquids | Week 2 onwards | Milk if tolerated; blended soups; smooth dahi drinks | Test dairy slowly. Stop if discomfort follows. |
| Stage 3: Soft or Pureed Foods | Week 3-4 | Soft dal, mashed potato, khichdi, pureed vegetables | Never force food. 4-6 small meals per day. |
| Stage 4: Soft Regular Foods | Month 2 onwards | Gradual return to soft regular foods over months | Chew thoroughly. Eat slowly. No large portions ever. |
Foods to actively avoid after esophagectomy: caffeine, alcohol, carbonated drinks, citrus fruits, spicy food, tomatoes, and peppermint. These cause significant discomfort while the esophagus and reconstructed stomach are healing.
Dumping syndrome is a real and very distressing complication that many esophageal surgery patients encounter for the first time without any warning. It happens when food moves too quickly from the reconstructed stomach into the small intestine.
Within 15 minutes of eating, you may experience nausea, cramping, sweating, and sudden diarrhea. Managing it is straightforward once you understand the rules: avoid sugary foods and refined carbohydrates entirely, eat your meals dry without liquids, and wait at least 30 to 45 minutes after meals before drinking any water or fluid.
Post-esophagectomy lactose intolerance is also common in the recovery period. Start with hard cheese and yogurt, which contain significantly less lactose than plain milk, and test your tolerance gradually over weeks.
Long-term after esophageal surgery, you will likely need supplementation for Vitamin B12, calcium, iron, and folic acid, since the body's ability to absorb these nutrients changes after surgery. Always review this with your surgical team at follow-up appointments.
According to research in BMC Pulmonary Medicine, between 32% and 39% of thoracic surgery patients develop pulmonary atelectasis after their operation. Atelectasis means sections of the lung collapse or fail to fully expand, which can lead to serious and life-threatening respiratory complications.
Structured breathing exercises significantly reduce this risk and speed up the overall recovery process. Yet most patients are discharged without any specific instruction on how to do them. Here are the three exercises that thoracic surgeons and pulmonary rehabilitation specialists rely on most:
Place one hand on your stomach and one hand on your chest. Breathe in slowly through your nose. Your belly should rise, not your chest. Exhale slowly through your mouth. Do 10 repetitions, three times a day. This exercise retrains the breathing muscles that thoracic surgery directly affects. It is the single most important breathing exercise for post-surgical lung recovery.
Inhale through your nose for a count of two. Then exhale slowly through lips that are gently pursed together, as if you are blowing on a hot cup of chai very slowly. The exhale should take twice as long as the inhale. This slows your breathing rate and significantly improves how well your lungs exchange oxygen, which is reduced after thoracic surgery.
Take a deep breath in. Without exhaling, take another smaller breath on top of it. Then another. After 4 to 5 stacked breaths, hold for 3 seconds, then exhale fully and completely. This gradually rebuilds lung capacity after surgery without putting excessive strain on the chest wall during healing.
A randomized controlled trial of 108 lung resection patients found that yoga breathing exercises, including pranayama techniques, produced significant improvement in shortness of breath, exercise capacity, and anxiety levels compared to patients who did not practice them. Start these exercises as soon as your surgeon permits, and ask your care team for a referral to a pulmonary rehabilitation specialist.
This is a risk factor that is particularly important for Indian patients and families, yet almost never discussed in mainstream cancer content. Cooking fumes from biomass fuels, the repeated high-temperature heating of oils, and poor kitchen ventilation release carcinogenic compounds including Benzo[a]pyrene. This compound directly alters the balance of gut bacteria and damages lung tissue over time, according to research in Frontiers in Nutrition (2024). Non-smoking women who cook over solid fuels in poorly ventilated kitchens are among the highest-risk groups for lung cancer in India.
Simple steps to reduce indoor air exposure at home:
Poor sleep raises cortisol levels in the body. High cortisol creates a biological environment that actively supports tumor growth. Sleep deprivation also damages gut bacteria, which as we have already seen, directly weakens the immune protection of your lungs. Thoracic cancer patients with untreated sleep disorders consistently show worse treatment tolerance than those who sleep well.
Practical steps that work: maintain a consistent sleep and wake time every day including weekends, avoid phone and screen use after 9 pm, keep the bedroom cool, dark, and quiet.
Chronic stress triggers a biological cascade that suppresses the immune cells your body relies on to fight cancer. It also causes gut dysbiosis, which further weakens the gut-lung immune connection we have discussed. Yoga, walking in an open park, speaking with a counselor, and joining a cancer support group are all evidence-based methods for managing stress during both treatment and the recovery period.
Many people associate cancer risk exclusively with smoking and never consider alcohol. But alcohol is a proven carcinogen with a well-established and direct connection to esophageal cancer, which is among the more common thoracic cancers in non-smokers. Even regular moderate alcohol consumption raises cancer risk meaningfully. The World Health Organization and the American Cancer Society both state clearly that no level of alcohol consumption is safe from a cancer prevention standpoint.
Men need approximately 3.7 liters of fluid per day and women approximately 2.7 liters, with a significant portion coming from food. Dehydration after thoracic surgery causes fatigue, dry mouth, and nausea, all of which are frequently misread as treatment side effects when they are actually a fluid problem. After esophageal surgery in particular, sip water consistently in small amounts rather than drinking large volumes at once. Coconut water, ORS, and diluted fruit juices help rehydration on days when plain water is not appealing.
The goal is not a perfect diet or a rigid exercise schedule. The goal is a consistent set of small habits that build on each other over time and become part of how you live.
Start with one change per week. Add a bowl of dahi to your lunch. Replace one packaged snack with a banana or a small handful of peanuts. Walk for 20 minutes after dinner. Practice 5 minutes of diaphragmatic breathing each morning before you check your phone. Over months, these small consistent actions build a foundation that supports your body through treatment and long-term recovery.
Think of movement the same way. Start with walking, even just short distances around the house in the early weeks after surgery. By week three or four, extend the distance gradually. By month two, introduce gentle stretching. Strength training and longer cardio sessions come later, always with your doctor's explicit clearance.
And always remember: mental health is physical health. Joining a support group, speaking with a counselor regularly, and staying connected with people who care about you are all genuine parts of thoracic cancer recovery. They are not optional extras.
Every patient's situation is different. What works nutritionally for one person may not be appropriate for another, depending on their specific cancer type, treatment stage, and surgical history. This guide gives you the knowledge to ask better questions and make more informed choices, not to replace your medical team.
If you or someone in your family is navigating a thoracic cancer diagnosis, whether exploring stage 4 lung cancer treatment in Gurgaon, considering Thoracic Surgery in Delhi, or looking for a trusted oncologist in Gurgaon for a second opinion, Dr. Parveen Yadav and the team at Chest Surgery India provide comprehensive thoracic surgical care that goes well beyond the operating room. This includes personalized guidance on nutrition, prehabilitation, and post-surgical recovery for every patient.
Free Second Opinion Available. Submit your reports and receive a specialist response within 48 hours. Visit chestsurgeryindia.com to connect with the team.
The operating room is where surgery happens. But the work of recovery and the work of prevention happen in your everyday life. If you could make one honest change to your diet, your sleep, or your daily habits starting tomorrow, what would that one change be? It might matter far more than you realize.

18+ Yrs Exp | 5,700+ Thoracic & Robotic Cancer Surgeries
Dr. Parveen Yadav is a Director and Senior Consultant in Thoracic and Surgical Oncology, specializing in minimally invasive and robotic lung and esophageal surgeries, with advanced training from AIIMS and Tata Memorial Hospital.
View Full ProfileDiscover how Da Vinci robotic surgery is transforming chest procedures in Gurgaon. Less pain, faster recovery & expert care by a certified thoracic surgeon
Just diagnosed with thoracic cancer? Learn critical first steps, biomarker testing, and what to do in the first 2 weeks from expert Dr Parveen Yadav.
Learn how advanced robotic surgery treats thymoma and esophageal cancer with greater precision, minimal invasion and improved recovery beyond lung-focused care.
Copyright 2026 © Dr .Parveen Yadav all rights reserved.
Proudly Scaled by Public Media Solution!