
A diagnosis of lung cancer is a life-altering moment. It's a moment that often brings a wave of fear, uncertainty, and a confusing new vocabulary. You may be hearing terms like "thoracotomy," "VATS," "lobectomy," and "RATS," all while trying to answer one simple, urgent question: "What is the safest and best path to a cure for me?"
My team and I understand this. As a thoracic surgeon specializing in Lungs Cancer Treatment for over 18 years, my primary goal is to provide that clarity.
For decades, the "best" treatment was an extensive, open-chest surgery. Then, in the 1990s, a "keyhole" surgery called VATS (Video-Assisted Thoracic Surgery) became a revolutionary, less painful option. But technology and standards in medicine never stand still.
Today, that standard has evolved again.
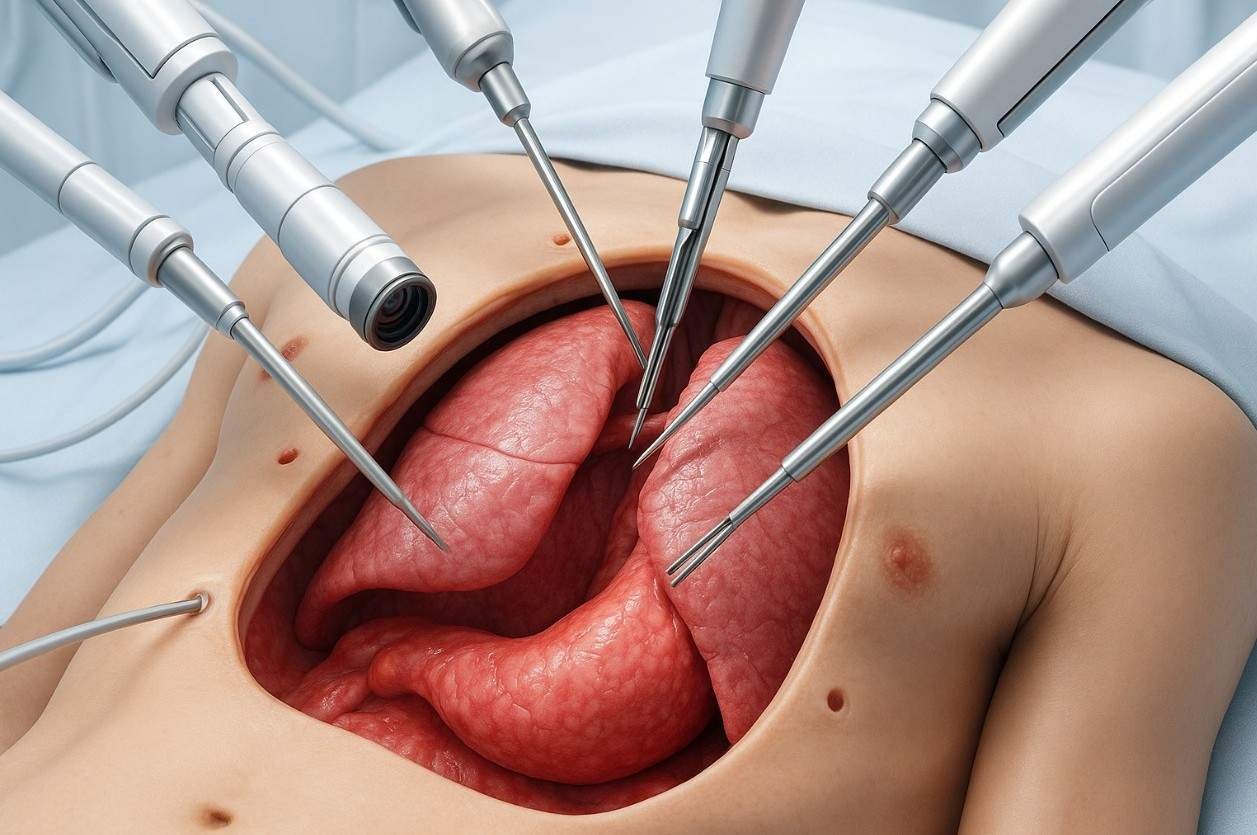
A quiet revolution has taken place, merging advanced technology with surgical expertise. It’s called Robotic-Assisted Thoracic Surgery (RATS), and it has set a new, higher standard for lung cancer surgery.
Robotic-Assisted Thoracic Surgery (RATS) is an advanced, minimally invasive procedure. A surgeon, in 100% control, uses a sophisticated robotic platform (like the da Vinci system) to operate through tiny incisions with 3D-HD vision and hyper-flexible, wristed instruments.
This article is the clear, factual guide you're looking for. We will explain precisely what RATS is, debunk the common myths, and detail the 7 evidence-based patient benefits that make it the new standard of care.
First, let's clear up the single biggest misconception.
Let me be perfectly clear: The robot does not perform your surgery. It is not autonomous, and it cannot make a single decision or movement on its own.
The da Vinci robotic system is an incredibly advanced tool that I control 100% of the time. Think of it as a $2 million extension of my eyes and hands, allowing me to perform complex operations with a level of precision that is simply not possible with other methods.
Here is how it actually works:
This system allows a surgeon to perform incredibly delicate work—like separating tiny blood vessels or removing cancerous lymph nodes from around the heart—through a few incisions smaller than your fingernail.
To understand why RATS is the new standard, you must first understand what it’s being compared to.
Most experts agree that long-term cancer survival between VATS and RATS is often comparable when done by experts. So, if survival is similar, why is RATS the new standard?
Because "standard of care" isn't just about survival. It's about the entire patient experience: safety during the operation, the quality of the cancer removal, post-operative pain, and the speed of your recovery.
In these crucial metrics, the data is precise.
This is what that advanced technology actually means for you, the patient.
The primary goal of any cancer surgery is to remove 100% of the tumor with "clean margins" (called an R0 resection). The 10x magnified, 3D view and wristed instruments allow the surgeon to dissect cancerous tissue with millimeter precision, separating it from vital healthy tissue like the heart, major blood vessels, and nerves. This unmatched precision gives you the absolute best chance of getting all the cancer out in a single operation.
This is the most critical oncological benefit and a key reason RATS is superior to VATS.
Surgery is not just about treating the cancer; it's also about staging it. We must remove the lymph nodes in the middle of your chest (the mediastinum) to see if the cancer has spread. This staging is critical; it's what tells your medical team if you need follow-up chemotherapy or immunotherapy to be cured.
This is where RATS truly excels. The 3D vision and wristed instruments allow the surgeon to perform a more thorough and complete lymph node dissection, retrieving more nodes from more stations.
What this means for you: A more accurate stage. Better staging means a more personalized and effective treatment plan. RATS gives your oncologists the best possible data to guide the rest of your Lungs Cancer Treatment and give you the best shot at a long-term cure.
The 3D-HD view allows your surgeon to see and meticulously seal even the tiniest blood vessels.
What this means for you:
This is a critical, often-unspoken patient risk, and a significant reason RATS is the new standard.
Sometimes during a minimally invasive VATS procedure, a surgeon encounters a challenge—like difficult scar tissue or unexpected bleeding. With 2D vision and rigid tools, they may not be able to control the situation and are forced to "convert" to a massive, traumatic open-chest surgery to finish the operation safely. This is essentially a "failed" keyhole surgery.
The 3D vision and wristed instruments of RATS give the surgeon the ability to handle these exact same challenges safely through the tiny incisions.
The 2024-2025 data is striking. Studies show RATS has a dramatically lower conversion rate.
What this means for you: RATS is the most reliable and predictable minimally invasive approach. When you are scheduled for a robotic keyhole surgery, you have the highest possible chance of it staying a keyhole surgery.
The primary source of pain after chest surgery is not the skin incision. It is the trauma of forcibly spreading the ribs apart.
Both VATS and RATS completely avoid this, which is why they are both far less painful than open surgery. However, RATS often results in even less pain than VATS. This is because the robotic instruments are designed to pivot inside the chest, placing minimal pressure on the sensitive intercostal nerves between the ribs. VATS instruments, being rigid, often pivot at the incision site, which can irritate these nerves.
What this means for you: A more comfortable recovery with less need for strong narcotic pain medications.
Less trauma, less pain, and fewer complications all add up to one thing: you get to go home to your family sooner.
A typical hospital stay for open-chest surgery is 5 to 10 days or more. With RATS, the average hospital stay is often just 2 to 4 days.
This is the ultimate goal. Recovery isn't just about leaving the hospital; it's about getting your life back.
Because your core muscles are not cut and your ribs are not spread, your body's energy is spent healing the lung, not recovering from massive trauma.
This table summarizes the key patient differences based on 2024-2025 data.
| Feature | Traditional Open Thoracotomy | VATS (The "Good" Standard) | RATS (The "New" Standard) |
| Incision | 1 large 8–10 inch incision | 2–4 small 1-inch incisions | 3–5 tiny 8mm–12mm incisions |
| Rib Spreading | Yes (severe trauma) | No | No |
| Surgeon's Vision | 2D naked eye | 2D flat-screen monitor | 3D-HD, 10x magnified console |
| Instruments | Human hand | Rigid, "chopstick-like" | Wristed, 360° rotation |
| Blood Loss | High | Low | Lowest |
| Conversion Risk | N/A | Higher (7.4% – 28.2%) | Drastically Lower (0.7% – 7.5%) |
| Lymph Node Removal | Good | Good | Superior / Most Thorough |
| Hospital Stay | 5–10+ days | 3–5 days | 2–4 days |
| Recovery Time | 2–3 months | 4–6 weeks | 2–3 weeks |
Here is the final, powerful proof that RATS is the new standard. A standard of care isn't just about being better at simple cases; it's about its ability to handle complex cases that the old standard (VATS) struggled with.
As medicine advances, many patients receive neoadjuvant (pre-surgical) chemo-immunotherapy. This treatment is highly effective at shrinking tumors, but it also causes dense scar tissue (fibrosis) in the chest, making the subsequent surgery notoriously difficult.
For a surgeon using 2D VATS, this scarred, woody tissue is incredibly challenging to dissect. In fact, studies on VATS after neoadjuvant therapy show conversion-to-open rates as high as 54%.
This is where RATS shines. The 3D vision and wristed instruments are uniquely suited to navigate this difficult scar tissue. Studies on RATS in these exact same patients show a low conversion rate, with some as low as 4.5%. This means patients who were previously told they must have open surgery can now get a minimally invasive RATS procedure.
The RATS platform gives surgeons the flexibility to tackle tumors in challenging locations, such as those deep in the center of the chest (near the heart) or at the very top of the lung (Pancoast tumors). The robotic "hands" can work around corners in ways that rigid VATS tools simply cannot, allowing for a complete resection in the tightest of spaces.
It is entirely normal to have questions. Here are the most common ones I hear in my clinic.
A: No, absolutely not. This is the most common myth. I am in 100% control of every movement, every second of the operation. The robot is an advanced tool, not an autonomous surgeon.
A: This is an important, practical question. The initial procedure cost of RATS is higher because the robotic technology and instruments are expensive.
However, most experts agree you must look at the total value. This higher initial cost is often offset by:
When you factor in the clinical benefits, especially the lower conversion risk and more accurate staging we believe the value is undeniable.
A: VATS is an excellent procedure and a massive improvement over open surgery. An expert VATS surgeon can achieve fantastic results.
However, the 2024-2025 data clearly shows that RATS provides measurable, non-negotiable advantages in the key metrics that define a modern, patient-first surgery:
While long-term survival is similar , many experts believe this is because of factors like accurate staging, which RATS simply does more thoroughly.
The da Vinci robot is an incredible tool. But in the end, it is just a tool. It cannot replace judgment. It cannot replace skill. And it cannot replace experience.
A robot in the hands of a low-volume or inexperienced surgeon will not produce a good result. The most critical factor in your cancer outcome is, and always will be, the experience of your surgeon.
You should look for a dedicated, high-volume thoracic surgeon who is a master of both VATS and RATS. This ensures they can offer you the right operation for your specific cancer, not just the "only" operation they know how to do.
As a Da Vinci-certified robotic surgeon, with training from India's premier cancer institutions AIIMS and Tata Memorial Hospital and over 5,700 thoracic procedures performed, my team and I are dedicated to this new standard of care. We combine world-class expertise with world-class technology.
A lung cancer diagnosis demands clarity. You deserve to know all your options, and you deserve to feel 100% confident in your treatment plan.
Because I believe so strongly that every patient deserves this clarity, my team at Chest Surgery India offers a Completely Free, No-Obligation Second Opinion.
Let us review your scans and your case. We will provide you with a detailed, expert opinion so you can make an informed decision with confidence. You have nothing to lose and a world of clarity to gain. contact us for more information

18+ Yrs Exp | 5,700+ Thoracic & Robotic Cancer Surgeries
Dr. Parveen Yadav is a Director and Senior Consultant in Thoracic and Surgical Oncology, specializing in minimally invasive and robotic lung and esophageal surgeries, with advanced training from AIIMS and Tata Memorial Hospital.
View Full Profile Pain After Thoracic Surgery: Tips for Smooth Recovery
Pain After Thoracic Surgery: Tips for Smooth Recovery
 Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
 Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures
Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures
Struggling with pain after chest surgery? Dr. Parveen Yadav shares expert recovery tips, causes of shoulder pain, PTPS signs, and what your discharge sheet won't tell you.
Discover how diet, breathing exercises & daily habits help prevent and recover from thoracic cancer. Expert insights from Dr. Parveen Yadav, Chest Surgery India
Discover how Da Vinci robotic surgery is transforming chest procedures in Gurgaon. Less pain, faster recovery & expert care by a certified thoracic surgeon
Copyright 2026 © Dr .Parveen Yadav all rights reserved.
Proudly Scaled by Public Media Solution!