
Hello, I'm Dr. Parveen Yadav. As a surgeon who specializes in complex thoracic procedures, I understand that receiving a diagnosis of esophageal cancer is a profound, life-altering event. When you are told you need an "esophagectomy," the world can feel overwhelming.
My goal with this guide is to clear away the confusion. I want to walk you through your surgical options, explain the modern techniques available, and give you a clear, honest look at the risks, benefits, and the road to recovery. This information is designed to empower you, so you can have a more informed conversation with your medical team and make the best possible decision for your unique situation.
At its core, an esophagectomy is a major surgery to remove part, or all, of the esophagus—the muscular tube that connects your mouth to your stomach. This operation is the primary surgical treatment for esophageal cancer.
After the cancerous portion of the esophagus is removed, the surgeon must reconstruct your digestive tract. In most cases, we do this by reshaping the upper part of your stomach into a tube, often called a "gastric conduit." This new, tube-shaped stomach is then carefully brought up into your chest and connected to the remaining, healthy part of your esophagus, allowing you to swallow.
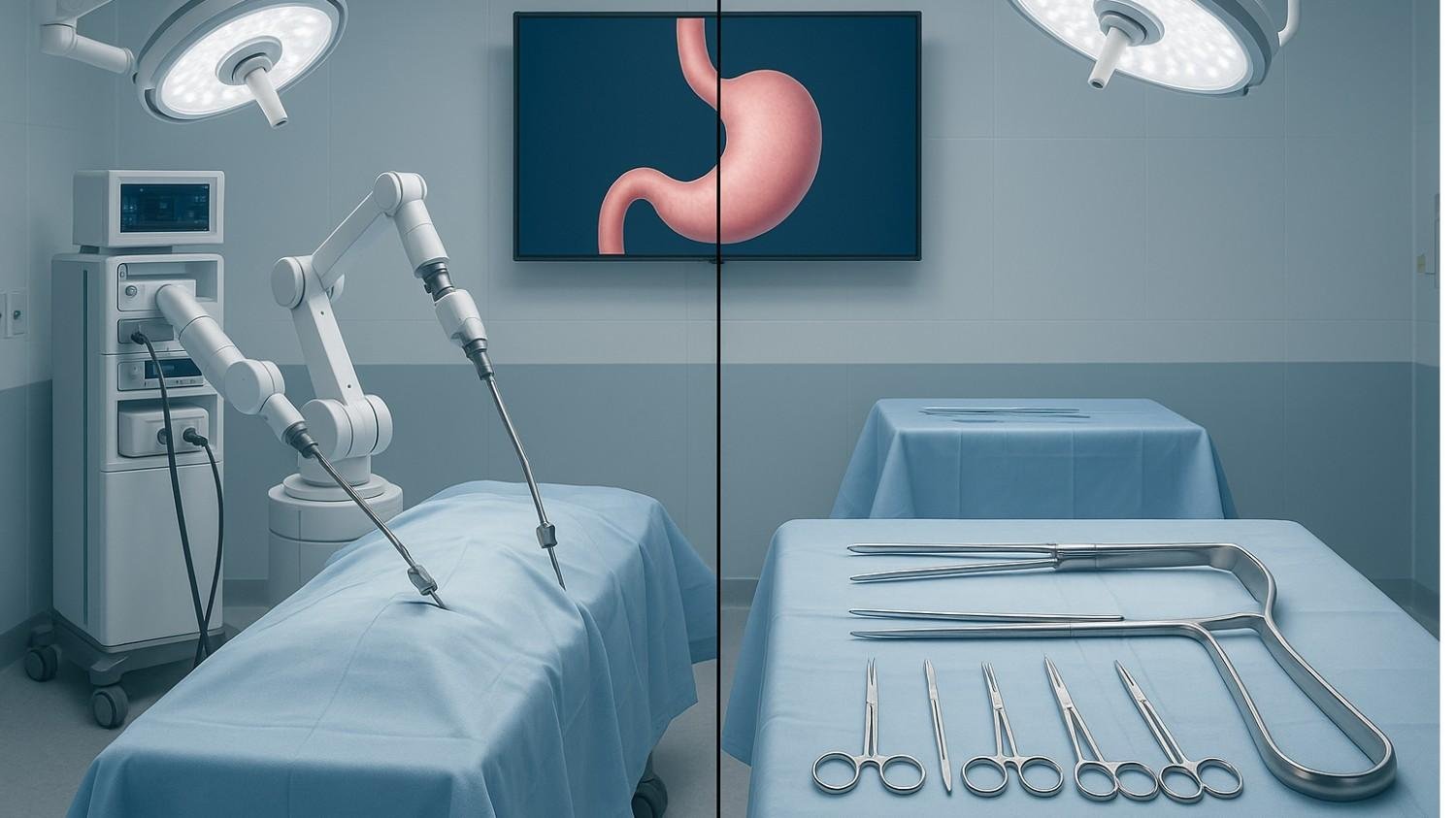
The fundamental operation removing the esophagus and rebuilding it is the same. The difference between "open" and "minimally invasive" is how the surgeon gets to the esophagus to perform the work. This difference in access has major implications for your recovery.
This is the conventional method that has been used for decades. It is defined by the use of one or more large incisions (cuts) to access your chest, abdomen, and sometimes your neck.
A key part of many open procedures is a thoracotomy, a large incision on the side of your chest that requires the surgeon to spread your ribs apart. This step, while providing wide access, is also a primary source of postoperative pain and is directly linked to a more increased risk of lung complications.
This modern approach avoids large incisions. Instead, your surgeon operates through several small "keyhole" incisions, each typically less than an inch long.
A tiny, high-definition camera is inserted through one of these small cuts, giving your surgeon a magnified view on a video monitor. The surgeon then uses long, thin, specialized instruments inserted through the other small cuts to perform the entire operation.
The most important difference for you as a patient is that MIE avoids the large, traumatic rib-spreading incision. This results in significantly less tissue damage, which is the primary reason it leads to less pain and, most importantly, fewer lung complications.
For nearly 25 years, MIE has been compared against the traditional open technique in major clinical trials. The evidence is now overwhelmingly clear.
| Feature | Minimally Invasive (MIE) | Open Esophagectomy (OE) |
| Incisions | Several small "keyhole" cuts | One or more large, long incisions |
| Rib Spreading | No | Yes (in most cases) |
| Post-Op Pain | Significantly Less | More significant pain |
| Blood Loss | Less blood loss | More blood loss |
| Lung Complications | Significantly Lower Risk | Higher Risk |
| Hospital Stay | Shorter | Longer |
| Cancer Removal | Equivalent | Equivalent |
| Long-Term Survival | Equivalent | Equivalent |
MIE has moved from an "alternative" to the "recommended standard" because it provides measurable, proven benefits to your recovery without compromising the cancer operation.
This is the most critical medical reason driving the shift to MIE. Lung complications, like pneumonia, are one of the most common and serious risks after an esophagectomy.
A formal 2024 consensus statement from surgical experts explicitly recommended MIE over open surgery to reduce the risk of pulmonary (lung) complications. The data is clear: MIE is associated with a 50% lower risk of major pulmonary complications.
This benefit is a direct result of the technique. The open thoracotomy (rib-spreading) causes significant trauma to the chest wall. This leads to severe pain, which makes it hard for patients to take deep breaths or cough effectively. This allows fluid to build up, which can lead to pneumonia. MIE's "keyhole" chest approach (VATS) avoids this specific trauma, breaking the chain that leads to lung complications.
MIE is simply a less traumatic operation for your body. This translates directly to your immediate recovery experience:
"Quality of Life" is a formal medical outcome that tracks your well-being. Studies show that MIE patients report a better quality of life at 6 weeks and even at 1 year, particularly in measures of physical function and pain. This means a faster return to feeling like yourself.
This is the number one question my patients ask, and it's the most important one. Does "minimally invasive" mean the cancer operation is "less effective"?
The answer, definitively, is no.
A common fear is trading a better recovery for a worse cancer outcome. The evidence from two decades of research overwhelmingly proves this is not the case. MIE is now considered the new gold standard precisely because it provides all the recovery benefits without compromising the cancer operation.
The two key goals of cancer surgery are to remove all the cancer (a "clear margin") and to remove enough lymph nodes to check for any spread.
This is the definitive answer. Multiple large-scale analyses and long-term follow-ups from major clinical trials have concluded there is no significant difference in 3-year or 5-year overall survival between patients who have MIE and those who have open surgery.
You get a safer, faster recovery with the exact same long-term chance of a cure.
To be transparent, any esophagectomy is a significant operation with serious risks. MIE is safer, but it is not risk-free.
MIE procedures consistently take longer than open surgery. An MIE can last 4 to 10 hours. This is not a disadvantage. This longer time is the process required to be meticulous, using small instruments and a camera, which is precisely what buys you the payoff of less tissue trauma, less blood loss, and fewer lung complications.
This is a leak at the new connection (anastomosis) between your stomach tube and your remaining esophagus. It is one of the most serious complications of this surgery. However, large-scale studies have concluded that there is no statistically significant difference in the rate of anastomotic leaks between the MIE and open groups.
The recurrent laryngeal nerve (RLN) is a delicate nerve that controls your vocal cord. It can be injured during the lymph node dissection, leading to hoarseness or swallowing difficulties. This risk is inherent to the dissection, and most studies find the risk to be similar between standard MIE and open surgery.
Robotic-Assisted Minimally Invasive Esophagectomy (RAMIE) is the most advanced type of MIE. The operation is still done through small keyholes, but the surgeon seats at a console controlling automatic arms.
The robot is a tool that enhances the surgeon's abilities. It provides :
This is where RAMIE truly shines. That delicate vocal cord nerve (RLN) is notoriously challenging to dissect around. Data now suggests that the robot's superior 3D vision and precision may lead to lower rates of vocal cord injury compared to both open and conventional MIE.
This is not a one-size-fits-all decision. Your surgical team will recommend the best and safest approach for you.
We evaluate many factors, including :
Initially, MIE was only for the "healthiest" patients. That has completely changed. Because MIE is a gentler, less traumatic procedure, it is now often the preferred option for patients who are considered higher risk for open surgery, such as elderly patients and patients with pre-existing lung disease (like COPD)
An open approach may still be recommended for patients with very large, bulky tumors, extensive cancer in the lymph nodes, or significant scar tissue from previous major surgeries.
This is a point I cannot stress enough. Esophagectomy is one of the most complex operations in surgery. MIE, in particular, is technically demanding and has a very steep learning curve.This means your outcome—your risk of complications—is heavily dependent on the expertise of your specific surgeon and their entire team. An experienced open surgeon at a high-volume center is a safer choice than an inexperienced MIE surgeon at a low-volume center.
Studies clearly show that outcomes for esophagectomy are significantly better at "high-volume centers"—hospitals that perform many of these operations every year.
This is why this complex surgery is increasingly centralized at high-volume, specialized centers. Think of it this way: just as a patient recovering from a complex stroke would be sent to a dedicated neuro rehabilitation centre in pune for highly specialized care, a patient undergoing an esophagectomy needs a team of surgeons, nurses, dietitians, and therapists who handle these specific, complex recoveries every single day.
Recovery is a marathon, not a sprint. MIE makes the initial phase safer and more tolerable, but the overall adjustment will take time.
You will not be able to eat or drink for the first several days to protect the new connection as it heals. During surgery, a feeding tube (J-tube) will be placed in your small intestine. This is how you will get all your nutrition. You will likely go home with this tube, and it is essential for your healing.
This is a critical concept. The short-term benefits of MIE (less pain, fewer lung issues) are related to the surgery. The long-term side effects are a consequence of the esophagectomy itself—the fact that your anatomy is permanently changed.
Acid reflux (GERD) is an unavoidable consequence of this operation. The surgery removes the body's natural anti-reflux barrier. This is not a failure of the surgery or the technique (MIE vs. Open); it is a known outcome of the reconstruction. This will be a lifelong focus, managed with lifestyle changes (like eating small meals and not lying flat after eating) and acid-suppressing medications.
Use this guide to have an empowered conversation. Do not be afraid to ask precise questions:
The evidence is clear: for the vast majority of patients, a Minimally Invasive Esophagectomy (MIE) offers a safer, faster, and gentler recovery with the exact same long-term cancer cure rate as a traditional open operation.
But the most important decision you will make is not which technique, but who performs it. Your choice of an experienced surgeon and a high-volume specialty center is the single most important factor in ensuring a safe operation and a successful recovery.
I hope this guide has provided you with clarity and confidence as you take the next step.

18+ Yrs Exp | 5,700+ Thoracic & Robotic Cancer Surgeries
Dr. Parveen Yadav is a Director and Senior Consultant in Thoracic and Surgical Oncology, specializing in minimally invasive and robotic lung and esophageal surgeries, with advanced training from AIIMS and Tata Memorial Hospital.
View Full Profile Pain After Thoracic Surgery: Tips for Smooth Recovery
Pain After Thoracic Surgery: Tips for Smooth Recovery
 Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
 Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures
Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures
Struggling with pain after chest surgery? Dr. Parveen Yadav shares expert recovery tips, causes of shoulder pain, PTPS signs, and what your discharge sheet won't tell you.
Discover how diet, breathing exercises & daily habits help prevent and recover from thoracic cancer. Expert insights from Dr. Parveen Yadav, Chest Surgery India
Discover how Da Vinci robotic surgery is transforming chest procedures in Gurgaon. Less pain, faster recovery & expert care by a certified thoracic surgeon
Copyright 2026 © Dr .Parveen Yadav all rights reserved.
Proudly Scaled by Public Media Solution!