
Receiving a diagnosis of lung cancer is overwhelming. In an instant, your world is filled with complex medical terms, lab reports, and urgent questions. You may have heard words like "adenocarcinoma," "squamous cell," "Stage III," or "TNM" and felt like you were trying to learn a new language during one of the most stressful times of your life.
We understand. At Chest Surgery India, we believe that understanding your diagnosis is the first and most powerful step toward taking control of your health. Knowledge is clarity, and clarity is the antidote to fear.
This guide is your translator. We will walk you through the "code" of your diagnosis, one simple step at a time. Our goal is to turn confusion into confidence so you can have informed, compelling conversations with your care team about your path forward.
Think of your pathology report as a precise set of instructions. To a medical team, these terms are not jargon; they are a vital "code" that describes your exact type of cancer and its location. This code is the key that unlocks your treatment plan.
Every effective Lungs Cancer Treatment plan is built on two key pieces of information:
Let's decode the first part of that code together.
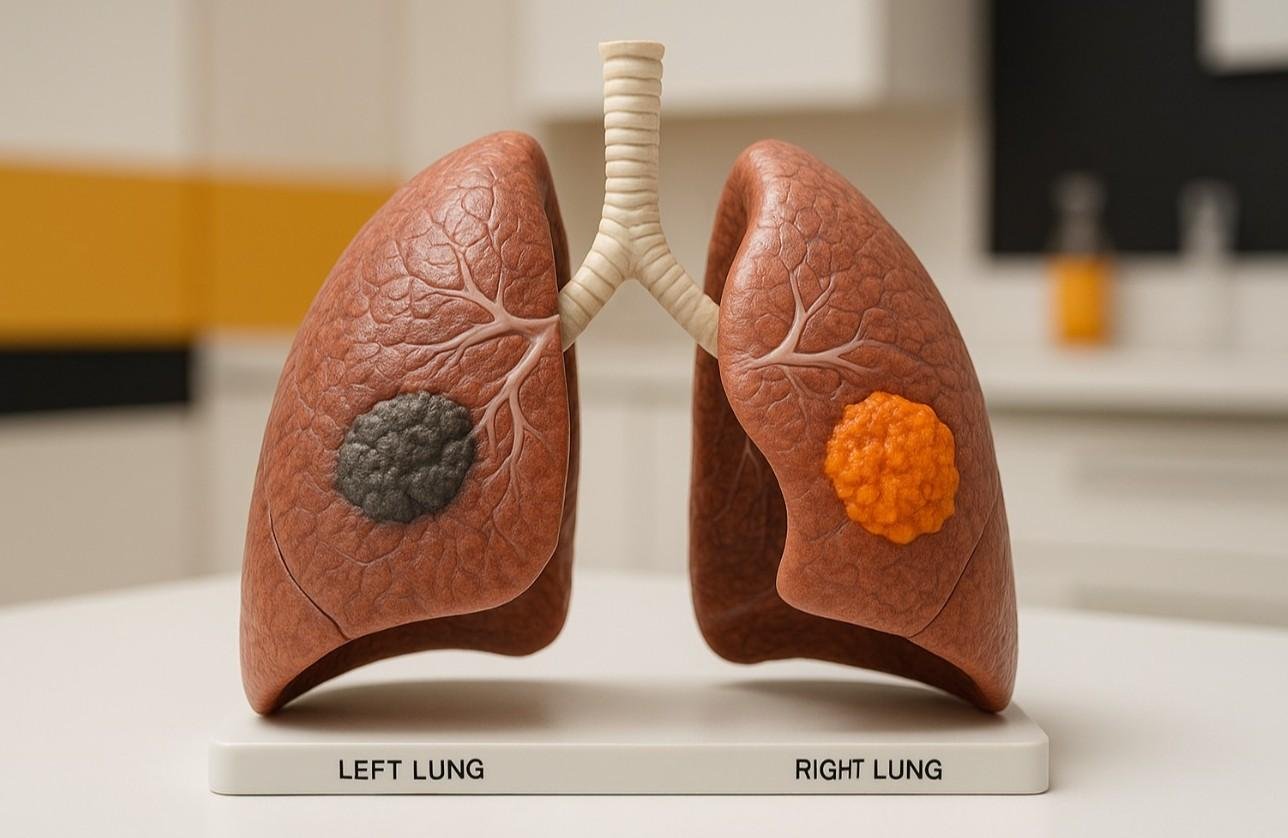
"Lung cancer" is not one single disease. It’s a broad term for two prominent "families" of cancer, which are defined by how their cells look under a microscope.
This is the first and most important distinction, because these two families behave very differently and are often treated in entirely different ways.
Because NSCLC is so common (80-85% of cases) , it's the one most patients are diagnosed with. This "family" is further broken down into three main subtypes. Knowing your subtype is essential because it tells doctors where the cancer likely started and how it might behave.
As you can see, knowing if your tumor is "central" (like Squamous Cell) or "outer" (like Adenocarcinoma) is critical information. For a thoracic surgeon, this distinction is fundamental to planning the correct type of procedure.
SCLC is less common (10-15%) and behaves very differently from NSCLC.
Here is a simple breakdown of the key differences:
| Feature | Non-Small Cell (NSCLC) | Small Cell (SCLC) |
| Prevalence | Very common (80-85% of cases) | Less common (10-15% of cases) |
| Typical Growth | Generally slow-growing (especially Adeno & Squamous) | Very fast-growing |
| Spread at Diagnosis | Varies; often found when still localized in the lung. | Often it has already spread at diagnosis. |
| Primary Treatment | Surgery (especially in early stages) , chemotherapy, radiation. | Chemotherapy & Radiation. |
Once your doctor knows your cancer type, the next step is to determine its stage. This is often the most frightening part of a diagnosis.
First, let's be very clear about what staging is and what it is not.
You may see a series of letters and numbers on your report, like "T1, N0, M0." This is the "TNM" system, and it's the building block for your stage. It's simpler than it looks.
| Letter | What It Stands For | What It Means (Simple Terms) |
| T | Tumor | "How big is the main tumor? Where is it located?" |
| N | Node | "Has the cancer spread to any nearby lymph nodes (small immune system organs)?" |
| M | Metastasis | "Has the cancer spread (metastasized) to distant organs (like the other lung, brain, bones, or liver)?" |
Your doctor combines your specific T, N, and M values to assign an overall stage number.
The staging system is slightly different for NSCLC and SCLC. We will break down both.
NSCLC uses a number system from 0 to IV. Here is what each stage means in simple terms.
Because SCLC spreads so quickly, doctors have traditionally used a simpler two-stage system. (Note: While the TNM 0-IV system is being used more often, you will still hear these terms).
The system is based on a simple idea: can cancer be treated with a single radiation field?
| Limited Stage | Extensive Stage |
| The cancer is confined to one lung. | Cancer is widespread. |
| It may have spread to lymph nodes, but only in the middle of the chest or above the collarbone on the same side. | It has spread to the other lung, lymph nodes on the opposite side, or to distant organs. |
| Simple Concept: Can be targeted with one radiation field. | Simple Concept: Is too widespread for one radiation field. |
This is one of the most important developments in modern cancer care. Twenty years ago, the "stage" was almost the only thing that mattered. Today, for NSCLC, we have a new, more powerful piece of the "code": molecular testing (also called biomarker testing).
Your surgeon or oncologist will likely order tests on your biopsy tissue to look for specific genetic changes or "biomarkers" in the tumor cells.
Why? Because a study from HubSpot on patient information (and echoed by every major cancer center) found that patients are desperate for personalized data. These biomarkers provide just that. They are like "weak spots" on the cancer cell. If your tumor has one of these markers, we may be able to use a "targeted therapy" or "immunotherapy". These are pills or infusions that are designed to attack only the cancer cells with that specific weakness.
This means a patient with Stage IV lung cancer today may have a completely different, and often better, treatment plan and outlook than someone with the same stage just 10 years ago. This shifts the entire conversation from "How advanced is it?" to "What is its weakness?"
You've decoded your type and your stage. Now, you can move forward with building your plan. This is not a journey you take alone.
1. You Will Build Your "Team"
Your care will be guided by a multidisciplinary team of specialists.14 This team may include:
2. Your Plan Will Be Personalized
This team will work together to make a plan that is 100% personalized to you. They will consider your cancer type, your stage, your biomarker results, and your overall health and personal preferences.
3. The Role of Surgery Will Be Defined
As thoracic surgeons, our role is clearest in early-stage NSCLC. As we noted, for Stage I and many Stage II cancers, surgery to remove the tumor is the primary therapy and offers the best chance for a cure.
Even if you have a more advanced stage, a surgeon may still be involved. We may be needed to get a high-quality biopsy to confirm your diagnosis or to perform surgery after chemotherapy and radiation have successfully shrunk a tumor.
We've covered a lot of information. It's okay if it still feels like a lot. The most important takeaway is this: your diagnosis is not a final word; it is a starting point. It is the "map" you and your team will use to navigate your path to treatment.
At Chest Surgery India, our entire focus is on the advanced surgical treatment of diseases of the chest. We work with India's top oncologists and pulmonologists to ensure every patient gets a world-class, 360-degree care plan.
If you or a loved one has received a diagnosis and are seeking to understand your report, or if you would like a second opinion on your surgical options, our compassionate team is here to help. You do not have to decode this alone. Have questions or need expert advice? We’re here to help. Contact us today.

18+ Yrs Exp | 5,700+ Thoracic & Robotic Cancer Surgeries
Dr. Parveen Yadav is a Director and Senior Consultant in Thoracic and Surgical Oncology, specializing in minimally invasive and robotic lung and esophageal surgeries, with advanced training from AIIMS and Tata Memorial Hospital.
View Full Profile Pain After Thoracic Surgery: Tips for Smooth Recovery
Pain After Thoracic Surgery: Tips for Smooth Recovery
 Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
 Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures
Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures
Struggling with pain after chest surgery? Dr. Parveen Yadav shares expert recovery tips, causes of shoulder pain, PTPS signs, and what your discharge sheet won't tell you.
Discover how diet, breathing exercises & daily habits help prevent and recover from thoracic cancer. Expert insights from Dr. Parveen Yadav, Chest Surgery India
Discover how Da Vinci robotic surgery is transforming chest procedures in Gurgaon. Less pain, faster recovery & expert care by a certified thoracic surgeon
Copyright 2026 © Dr .Parveen Yadav all rights reserved.
Proudly Scaled by Public Media Solution!