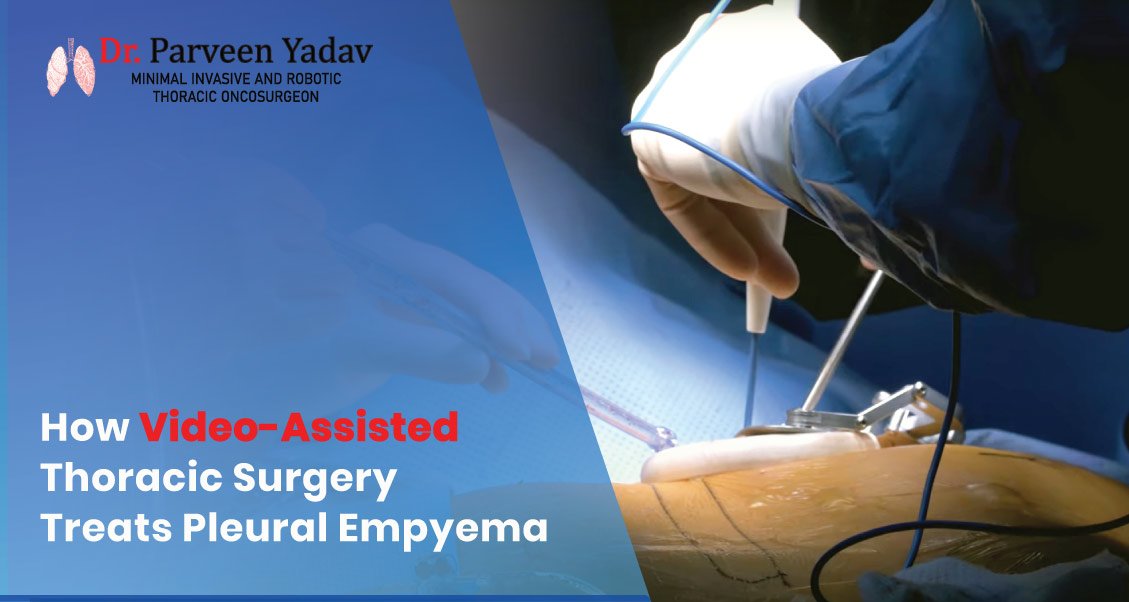
How Video-Assisted Thoracic Surgery Treats Pleural Empyema
-
Medically reviewed by
Dr. Parveen Yadav
18+ Yrs Exp | 5,700+ Thoracic & Robotic Cancer Surgeries
-
Nov 15, 2024
Pleural empyema, also known as empyema thoracis, happens when pus collects in the pleural cavity, the space surrounding the lungs. This condition often results from complications of bacterial pneumonia and can lead to severe respiratory problems, chronic infections, or even death if not treated effectively. Modern medical advances have introduced Video-Assisted Thoracic Surgery (VATS) as a transformative approach for managing pleural empyema, particularly in its advanced stages.
This blog comprehensively explains how VATS treats pleural empyema, delving into its methodology, advantages, outcomes, and comparisons with traditional surgical techniques.
Understanding Pleural Empyema
Pleural empyema, also known as empyema thoracis, is a serious medical condition in which pus collects in the pleural cavity—the thin fluid-filled space between the lungs and the chest wall. This accumulation is a result of an infection that spreads to the pleural space, most commonly bacterial pneumonia. If not treated promptly, pleural empyema can lead to severe complications, including respiratory failure, chronic infections, or death.
Causes of Pleural Empyema
The development of pleural empyema often begins with an infection in the lungs or chest. The most common causes include:
-
Post-Bacterial Pneumonia:
-
Mechanism: When pneumonia is inadequately treated or delayed, bacteria can penetrate the pleura, leading to pus formation.
-
Common Bacteria: Streptococcus pneumoniae, Staphylococcus aureus, and Klebsiella species are frequently implicated.
-
Post-Surgical or Post-Traumatic Infection:
-
Infections following thoracic surgery or penetrating chest injuries can introduce bacteria directly into the pleural cavity.
-
Spread from Other Infections:
-
Infections like tuberculosis or abscesses in nearby organs can invade the pleural space.
-
Aspiration or Esophageal Rupture:
-
Aspiration of stomach contents or esophageal injuries can lead to chemical irritation and infection.
Risk Factors for Pleural Empyema
Specific individuals are at a higher chance of developing pleural empyema due to predisposing conditions, including:
-
Chronic Medical Conditions:
-
Diabetes mellitus, kidney disease, and cancer can weaken the immune system, increasing infection susceptibility.
-
Immunosuppression:
-
Diseases like HIV/AIDS or the use of immunosuppressive drugs (e.g., corticosteroids or chemotherapy) make individuals more vulnerable to bacterial infections.
-
Delayed or Inadequate Treatment:
-
Failure to seek timely medical attention for respiratory infections can allow bacteria to spread unchecked.
-
Other Respiratory Diseases:
-
Disorders such as chronic obstructive pulmonary disease (COPD) or bronchiectasis can predispose individuals to empyema.
Pathophysiology of Pleural Empyema
The progression of pleural empyema occurs in three distinct stages:
Stage I: Parapneumonic Effusion
-
Description: In the early phase, sterile fluid builds up in the pleural cavity due to inflammation from pneumonia.
-
Key Characteristics:
-
There is no bacterial invasion yet.
-
Simple fluid collection that responds well to antibiotics and drainage.
-
Symptoms: Mild chest discomfort, fever, and cough.
Stage II: Fibrinopurulent Stage
-
Description: The infection progresses, and bacteria invade the pleural space, forming pus. Fibrinous septa (partitions) begin to develop, dividing the pus into loculated pockets.
-
Key Characteristics:
-
Presence of thick, infected fluid.
-
Fibrin deposits create barriers, complicating drainage.
-
Symptoms: Intense chest pain, high fever, difficulty breathing.
Stage III: Chronic Organizing Stage
-
Description: Scar tissue forms on the pleura, creating adhesions and trapping the lung, preventing it from expanding fully.
-
Key Characteristics:
-
Fibrous peel encases the lung.
-
Lung function is severely compromised.
-
Symptoms: Severe respiratory distress, chronic cough, and fatigue.
Symptoms of Pleural Empyema
The symptoms of pleural empyema can vary depending on its stage but generally include:
-
Persistent cough.
-
Difficulty breathing or shortness of breath.
-
Chest pain, especially during deep breaths.
-
High fever.
-
Chills and night sweats.
-
Fatigue and malaise.
-
Weight loss.
-
Severe breathing difficulties.
-
Reduced lung function due to trapped lung in stage III.
Diagnosis of Pleural Empyema
Timely diagnosis is critical for managing pleural empyema effectively. Diagnostic methods include:
-
Imaging Techniques:
-
Chest X-ray: Identifies pleural effusion but may not detect loculated fluid.
-
CT Scan: Provides detailed images of fluid pockets, septations, and lung involvement.
-
Ultrasound: Guides thoracentesis (fluid extraction) for diagnostic and therapeutic purposes.
-
Pleural Fluid Analysis:
-
Procedure: Thoracentesis is performed to extract fluid from the pleural cavity.
-
Analysis:
-
Presence of pus or turbid fluid.
-
High white blood cell count.
-
Positive bacterial cultures confirm infection.
-
Blood Tests:
-
Elevated white blood cell count.
-
Increased inflammatory markers include C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
Why Early Recognition is Important
If left untreated, pleural empyema can lead to severe complications, including:
-
Respiratory Complications:
-
Lung collapse (atelectasis).
-
Chronic respiratory failure.
-
Systemic Complications:
-
Sepsis: A life-threatening response to infection.
-
Multi-organ failure.
-
Chronic Illness:
-
Formation of fibrous tissue that permanently restricts lung expansion.
Stages and Treatment of Pleural Empyema
|
Stage
|
Characteristics
|
Treatment
|
|
Stage I
|
Inflammatory fluid collection, sterile
|
Antibiotics and drainage (chest tube or thoracentesis).
|
|
Stage II
|
Bacterial invasion, pus formation, loculations
|
VATS or chest tube drainage with antibiotics.
|
|
Stage III
|
Fibrous peel, lung entrapment
|
VATS or open thoracotomy decortication.
|
What is Video-Assisted Thoracic Surgery (VATS)?
VATS is a minimally invasive surgical technique that allows surgeons to treat pleural empyema through small incisions. Using a thoracoscope—a thin tube with a camera—surgeons can visualize the pleural cavity and perform procedures such as debridement (removal of infected tissue) and decortication (removal of fibrous adhesions).
How VATS Works
-
Small Incisions: Unlike traditional open thoracotomy, VATS requires only one to three minor cuts.
-
Enhanced Visualization: High-definition cameras provide clear views of the infected area.
-
Precise Instrumentation: Specialized tools are used for debridement and tissue removal.
Why Choose VATS for Pleural Empyema?
Benefits of VATS
-
Minimally Invasive Approach:
-
Smaller incisions reduce surgical trauma, pain, and scarring.
-
Patients recover faster and require shorter hospital stays compared to open thoracotomy.
-
Better Surgical Precision:
-
Surgeons can visualize infected areas, allowing effective removal of pus and fibrous tissue.
-
Improved accuracy in treating loculated fluid pockets.
-
Favorable Patient Outcomes:
-
Significant lung re-expansion occurs in more than 90% of patients.
-
Low postoperative complication rates.
-
Cosmetic results are ranked as good to excellent by most patients.
Supporting Data
|
Outcome Measure
|
VATS
|
Open Thoracotomy
|
|
Average Hospital Stay
|
8–10 days
|
12–15 days
|
|
Operative Time
|
~130 minutes
|
~150 minutes
|
|
Mortality Rate
|
<1%
|
~2%
|
|
Postoperative Pain (VAS Scale)
|
1.5–2.5/10
|
4–5/10
|
How Video-Assisted Thoracic Surgery Treats Empyema
Preoperative Preparation
Before surgery, patients undergo thorough assessments to ensure the best outcomes:
- Imaging:
- CT Scans: Identify fluid pockets, fibrinous septa, and lung entrapment.
- Ultrasound: Guides the surgical plan by revealing locations.
- Antibiotics:
- Broad-spectrum antibiotics are started to reduce infection.
- Targeted therapy follows once culture results identify the specific pathogen.
The VATS Procedure
- Anesthesia and Incisions:
- Patients are placed under general anesthesia.
- One to three small incisions are made to insert the thoracoscope and instruments.
- Debridement:
- Surgeons remove pus, necrotic tissue, and fibrinous septa that block lung expansion.
- Decortication:
- The fibrous peel encasing the lung is carefully removed to allow the lung to re-expand fully.
- Drain Placement:
- A chest tube removes residual fluid and air, preventing recurrence.
Postoperative Care
- Monitoring: Patients are monitored for complications such as bleeding or infections.
- Pain Management: Postoperative pain is managed effectively with minimal discomfort.
- Physiotherapy: Lung exercises are initiated to aid recovery.
Real-World Cases
Case 1: Advanced-Stage Empyema in a 60-Year-Old Male
A patient with stage III empyema underwent VATS for debridement and decortication.
- Procedure Duration: 135 minutes.
- Outcome: Lung re-expansion visible on postoperative imaging.
- Recovery: Discharged after 10 days with no recurrence at the 6-month follow-up.
Case 2: Middle-aged female with Stage II Empyema
A 45-year-old woman presented with loculated pleural fluid.
- Procedure Duration: 95 minutes.
- Postoperative Pain: Low (VAS score 2/10).
- Outcome: Complete recovery with no complications reported at 1-year follow-up.
Comparison: VATS vs. Open Thoracotomy Decortication
|
Parameter
|
VATS
|
Open Thoracotomy Decortication
|
|
Surgical Trauma
|
Minimal
|
Extensive
|
|
Hospital Stay
|
Shorter (8–10 days)
|
Longer (12–15 days)
|
|
Cosmetic Outcome
|
Better due to smaller incisions
|
Visible scarring
|
|
Suitability
|
Ideal for stages II and early III
|
Suitable for all stages, especially advanced cases
|
Limitations of VATS
- Challenges in Advanced Stages:
- Dense adhesions in stage III empyema may require conversion to open thoracotomy.
- Need for Expertise:
- VATS outcomes depend heavily on the surgeon's experience and skill.
- Study Gaps:
- Lack of large-scale randomized controlled trials (RCTs).
- Retrospective analyses may introduce bias.
The Future of Empyema Treatment
Technological Innovations
- Robotics: Robotic-assisted thoracic surgery (RATS) may enhance precision in complex cases.
- AI Integration: AI-driven imaging can help surgeons plan and execute procedures more effectively.
Research Directions
- Randomized controlled trials comparing VATS and open thoracotomy.
- Development of stage-specific treatment protocols.
Final Words
Video-assisted thoracic Surgery (VATS) has emerged as a breakthrough treatment for pleural empyema, particularly in stages II and III. Its minimally invasive nature reduces pain and scarring, shortens recovery time, and improves clinical outcomes. While open thoracotomy remains indispensable for advanced and complex cases, VATS has become the preferred first-line treatment option when performed by skilled surgeons.
Chest Surgery India is the best hospital for those seeking world-class care for thoracic conditions in Gurgaon, India. Equipped with advanced facilities and innovative technology, the hospital excels in treating pleural empyema and other thoracic conditions. Guided by the expertise of Dr Parveen Yadav, widely regarded as the best thoracic oncologist in the country, Chest Surgery India ensures optimal patient outcomes and personalized care.
Early diagnosis and timely intervention at a trusted institution like Chest Surgery India can make all the difference in recovery and quality of life for patients with pleural empyema. Consult with experts to explore the best treatment options tailored to your condition.
Dr. Parveen Yadav
18+ Yrs Exp | 5,700+ Thoracic & Robotic Cancer Surgeries
Dr. Parveen Yadav is a Director and Senior Consultant in Thoracic and Surgical Oncology, specializing in minimally invasive and robotic lung and esophageal surgeries, with advanced training from AIIMS and Tata Memorial Hospital.
View Full Profile


 Pain After Thoracic Surgery: Tips for Smooth Recovery
Pain After Thoracic Surgery: Tips for Smooth Recovery
 Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
Diet & Lifestyle for Thoracic Cancer Prevention | Dr. Parveen Yadav
 Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures
Robotic Thoracic Surgery: How Da Vinci Technology is Revolutionizing Chest Procedures